Vascular anomalies
2.5. PI3K-related overgrowth syndromes (PROS, PIK3CA Related Overgrowth Spectrum)
PI3K, AKT and PTEN: what are they?
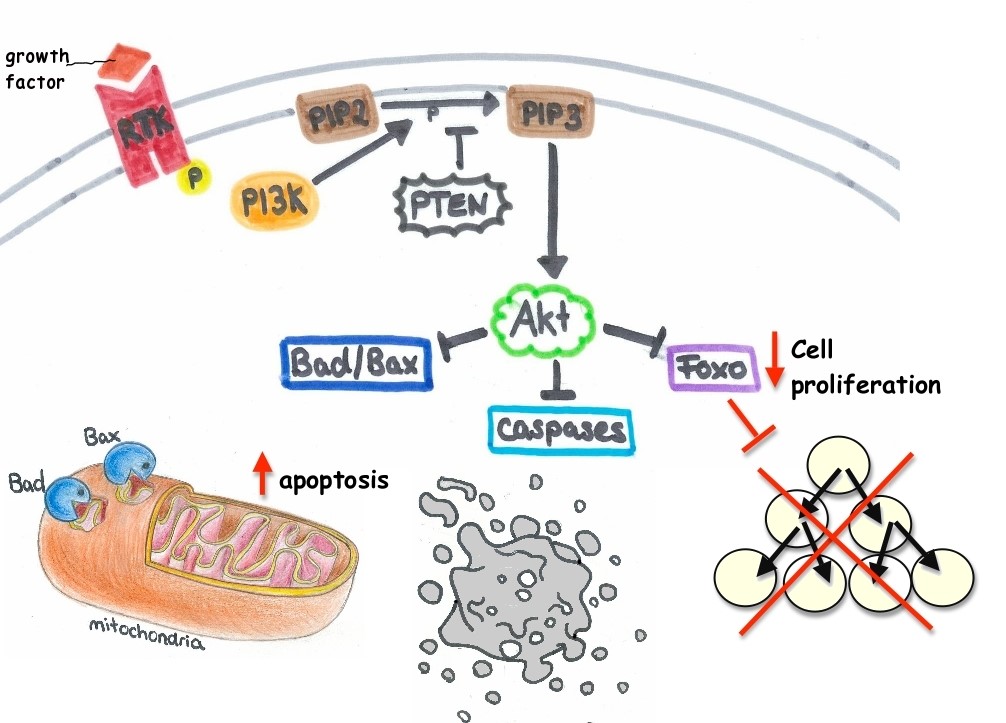
PI3K and AKT are two proteins that belong to the same intracellular signalling pathway and are responsible for many processes in response to extracellular signals, such as, regulation of the cell cycle, cell survival (sending cells into an inactive state, to senescence, or to continue with proliferation), cell growth, angiogenesis, etc.
PI3K is the abbreviated name of the molecule phosphoinositide 3-kinase (PI3K), one of the key signalling molecules in the intracellular signalling pathway PI3K-AKT (it does not function without it).
AKT, also known as protein kinase B (PKB), is another key molecule in the intracellular signalling of this pathway. It is activated by phosphorylation, and if the pathway works correctly, AKT is activated after PI3K.
Vascular malformations in children often show mutations in these two molecules, which affect the entire PI3K/AKT pathway.
PI3K is an oncogene, i.e., its activation triggers cell growth and proliferation. This means that a mutation can cause the overexpression of PI3K, which will lead to uncontrolled cell proliferation and growth. In addition, a mutation at any stage of this pathway (it does not necessarily need to be a mutation on PI3K) that causes overexpression, will likely trigger uncontrolled proliferation of cells.
PTEN is the last molecule in this pathway, and the PTEN gene is spread throughout our entire body due to its importance as a tumour suppressor gene. PTEN inhibits AKT activation by dephosphorylating PIP3 in PIP2, which means it counteracts the AKT signalling effect, and therefore, stops cell proliferation and cell growth. The mutation of this gene leads to its poor functioning, and as a consequence it causes loss of control over the cell cycle and tumours. Many tumours have mutations in the PTEN gene.
2.5.1. PROS: PI3K Related Overgrowth Spectrum
PROS, or PI3K Related Overgrowth Spectrum, is a spectrum (a group) of diseases that share the characteristic mutation in PI3K, which affects the PI3K/AKT pathway, leading to excessive growth.
There are many pathologies that can be considered PROS, such as megalencephaly-capillary malformation syndrome (MCAP), macrodactyly, CLOVES, fibroadipose overgrowth (FAO), and other rare syndromes. In all of these diseases, we can observe the excessive growth of body structures (to a greater or lesser extent), which can end up being life-threatening for the patient. Overgrowth can be found in intra and extracorporal tissues.
The PI3K/AKT cell signalling pathway is long as has many steps. The potential mutations in each one of the proteins along the pathway are different, although sometimes the difference is very subtle and the effect of the mutations is the same.
AKT (gene) can also experience mutations, which will lead to an overexpression of this protein and thus, an uncontrolled proliferation of affected cells. The following syndrome is the result of the mutation of AKT type 1 (AKT1).
2.5.1.1. Megalencephaly-capillary malformation syndrome
Megalencephaly-capillary malformation syndrome is characterised by the combination of capillary malformations and megalencephaly and another abnormal findings such as overgrowth, craniofacial and skeletal abnormalities, developmental delay, neurological abnormalities, intellectual disabilities and connective tissue disorders. Capillary malformations are often located in the centrofacial region (nose, glabella, and philtrum). The most common findings in skull X-ray studies are ventriculomegaly, megalencephaly, brain and/or cerebellar asymmetry, as well as herniation of the cerebellar tonsils.
2.5.1.2. CLOVES syndrome
CLOVES syndrome is an overgrowth syndrome characterized by increased fatty tissue at birth, as well as vascular malformations, epidermal nevi and skeletal and spinal abnormalities. Children with CLOVES syndrome may have increased fatty tissues, especially in the chest and the abdomen, with overgrowth even after removal. Vascular malformations can be high-flow and be located at the paraspinal level, with a risk of causing medullar damage. With regards to musculoskeletal abnormalities, these usually affect the hands and feet, although scoliosis, spina bifida, developmental dysplasia of the hip, pectus excavatum and rib abnormalities may also occur. These children may also have neurological anomalies, such as spasticity, paralysis or tethered cord syndrome. CLOVES syndrome has been associated to postzygotic mutations in the PIK3CA gene.
2.5.2. Proteus syndrome
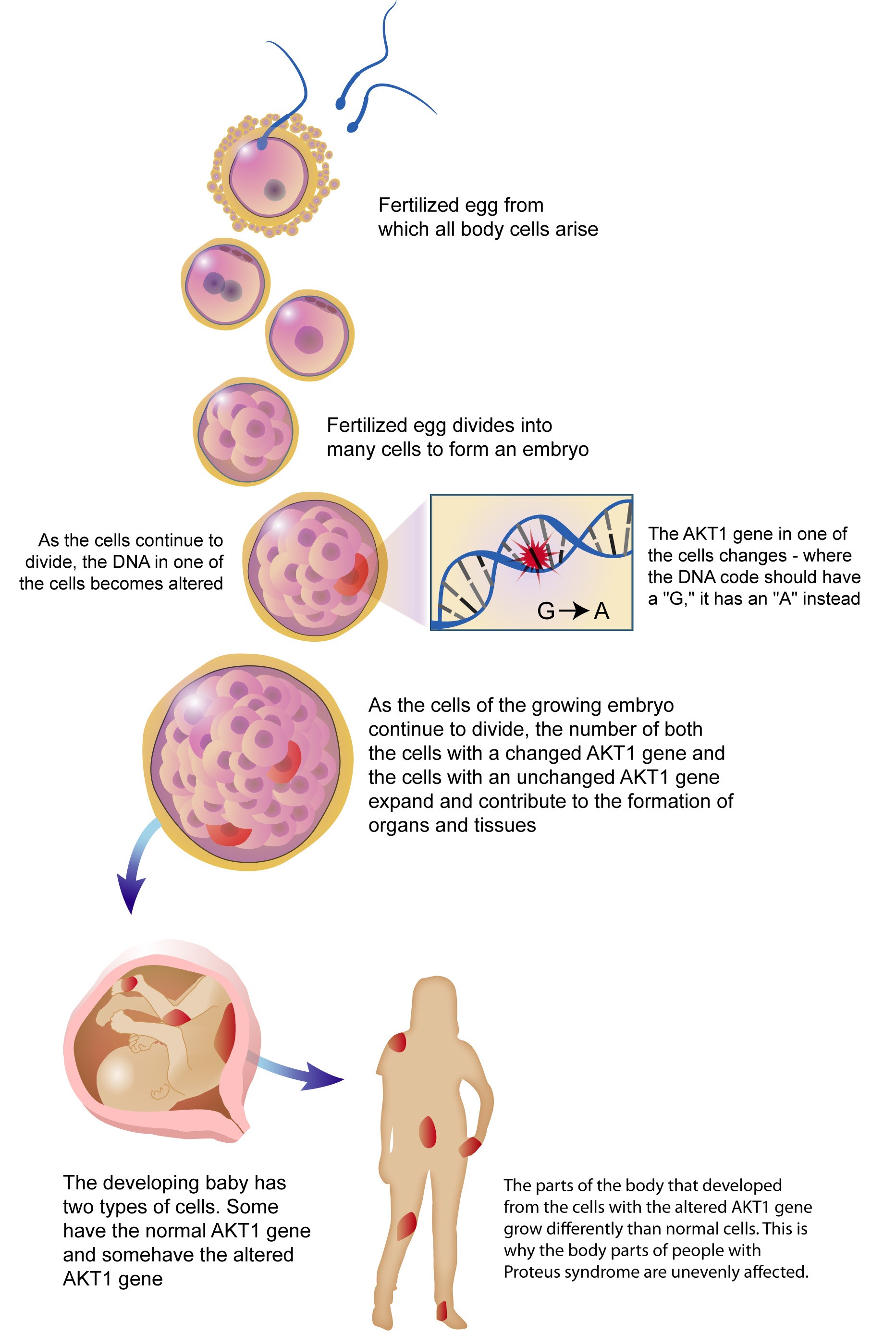
AKT is a key protein in the PI3K/AKT intracellular signalling pathway, and it has three different types of isoforms: AKT 1, 2 and 3. This syndrome has been linked to a mosaic activating mutation of AKT1 and has a prevalence of 1/1,000,000 in children and adults. A mosaic activating pattern means that the mutation may sporadically appear in some cells and not in others, and it is also implicit that it is NOT inherited.
The cells with the mutation will start to proliferate and accumulate cells with the mutation, just like the "parent" cell, which will result in the characteristic disorders of this syndrome.
Proteus syndrome is described as a rare overgrowth syndrome that usually affects the skin. Excessive growth is seen mainly in the skin, the bones and other tissues, such as the endothelium ,and it generally grows asymmetrically. Overgrowth becomes more serious with age and it is not visible in newborns. It is visible from the age of 6–18 months.
Main effects
Bone overgrowth is the most visible effect due to the severe deformities it causes. The limbs, the cranium and the spinal column are the most affected bones.
The skin may show a great variety of growths. The most common is CCTN (cerebriform connective tissue nevus), which is defined as a thick and elevated injury with deep groves and that generally occurs on the soles of the feet. Assessing the progression of skin lesions in these patients is carried out using the CCTN score and growth rate.
Blood vessels may also be affected by the excessive growth. The involvement of blood vessels is the origin of vascular malformations in Proteus syndrome.
Possible complications
The main complications of Proteus syndrome are the development of benign tumours (in any tissue), especially in adipose tissue, and deep vein thrombosis (DVT). DVT are blood clots formed due to slow blood flow in the deep veins of legs and arms. Parts of these blood clots may travel directly via the bloodstream to the heart and lungs, where they can generate an obstruction and cause a pulmonary embolism, which is a potentially fatal condition. This is a common cause of death in people with Proteus syndrome.
It is particularly important to provide a differential diagnosis with other diseases similar to these kind of overgrowth symptoms, as they are clinically difficult to distinguish. Proteus syndrome tends to be over-diagnosed.
Associated genetic defects
As previously mentioned, Proteus syndrome results from a mutation in the AKT1 gene. It is not inherited and occurs randomly in a cell during the first stages of development before birth (embryonic period). AKT1 regulates cell growth, cell division and cell death. Mutations make the cell grow and divide abnormally. The increase in cell proliferation in the tissues results in abnormal growth, characteristic of Proteus syndrome. These mutations are more common in cell types with a high proliferation rate (such as the skin or blood cells), rather than in tissues that have a normal growth rate or with no proliferation at all, such as neurons or cardiomyocytes.
The mutation of the PTEN gene, which is responsible for the synthesis of the PTEN protein, has also been linked to Proteus syndrome. However, these patients do not meet the strict criteria for the diagnosis of this syndrome.
It is important to bear in mind that these genetic disorders are NOT inherited, so it is not necessary to look at the family genes when searching for the mutation.