Vascular anomalies
2.4. Arteriovenous malformations (AVMs)
AVMs are abnormal connecting arteries and veins. They are all pathological and rapid blood flow malformations. AVMs are the most dangerous type of malformation because they block tissue oxygenation. When blood passes directly from the arteries to the veins, it does not reach the capillaries and consequently, there is no exchange of oxygen and CO2 between the tissues and the blood. Therefore, the blood returns to the heart carrying the oxygen that was meant to oxygenate the tissues, causing the following clinical symptoms: cyanosis, fatigue, ulceration, haemorrhagia, necrosis, cardiac decompensations, etc. AVMs may occur in many parts of the body and progress over time, meaning that some AVMs will have more serious clinical manifestations than others.
To diagnose AVMs we use the Schobinger staging system, which classifies patients according to the clinical symptoms they have. This staging is progressive: it is not possible to have stage 3 AVM without having gone through stages 1 and 2, for example.
- Stage 1 (Quiescence): patients with reddish capillary injuries which may slightly infiltrate into the dermis and may feel warm. This tends to be the first manifestation of an AVM. These macular injuries are very similar to those in Parkes Weber syndrome.
- Stage 2 (Expansion): growth phase of the AVM area. The area enlarges due to the expansion of the vein (the artery supplies a much bigger flow than the vein is used to so it expands), the blood adquires a turbulent (not laminar) flow, which is why a murmur can be heard when the blood passes through. Pulsations may also appear in the AVM area.
- Stage 3 (Destructive/Dystrophic changes): ulcerations may appear in the tissue surrounding the AVM, which may cause bleeding and necrosis. Lytic bone lesions may also occur.
- Stage 4 (Decompensation): the patients in this stage have congestive heart failure due to the excess blood that returns to the heart.
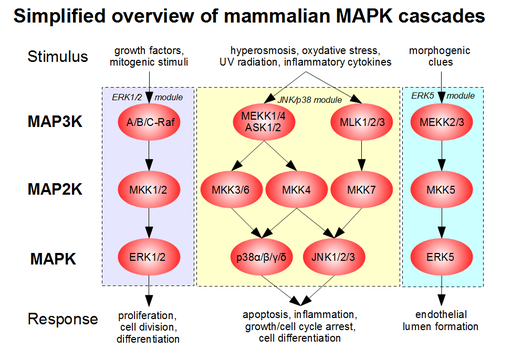
Most AVMs are the result of sporadic mutations, which means that they appear after the child is born. We know that these mutations appear in very specific sites of the genome known as “hot spots”. These are locations that are more susceptible to mutations than others. One of these locations is found in the genes that are in charge of synthesising MAP kinase proteins. Knowing this, we can develop therapies with drugs that block the transcription of these genes (MAP or BRAF inhibitors).
Other forms of the disease are AVMs associated with syndromes such as the Parkes-Weber syndrome (Section 2.1.2.) or Cobb syndrome.
2.4.1. Cobb syndrome
Cobb syndrome is a very rare disease developed due to spontaneous mutations and is characterised by skin, vertebral and intramedullary AVMs and in a few cases, meningeal AVMs. These AVMs appear along the same myelomere (fragment of the spinal cord that contains both the afferent and efferent components of a nerve root).
Currently, the most plausible theory is that these abnormalities appear due to mutations in a group of genes known as RASA1.
Patients with Cobb syndrome tend to present with reddish/brownish stains in the AVM area, which are usually diagnosed in stage 1 or 2. Neurological symptoms typically appear throughout adolescence, which may vary from back pain to paraparesis and paraplegia. These symptoms appear due to the compression AVM causes on the spinal cord (or on the cerebral cortex in the case of it being in the meninges), blocking the nerve impulse.
Symptoms and prognosis can impove if we reduce the size of AVMs through endovascular embolisation.