Epidermolysis bullosa
2. Ophthalmology
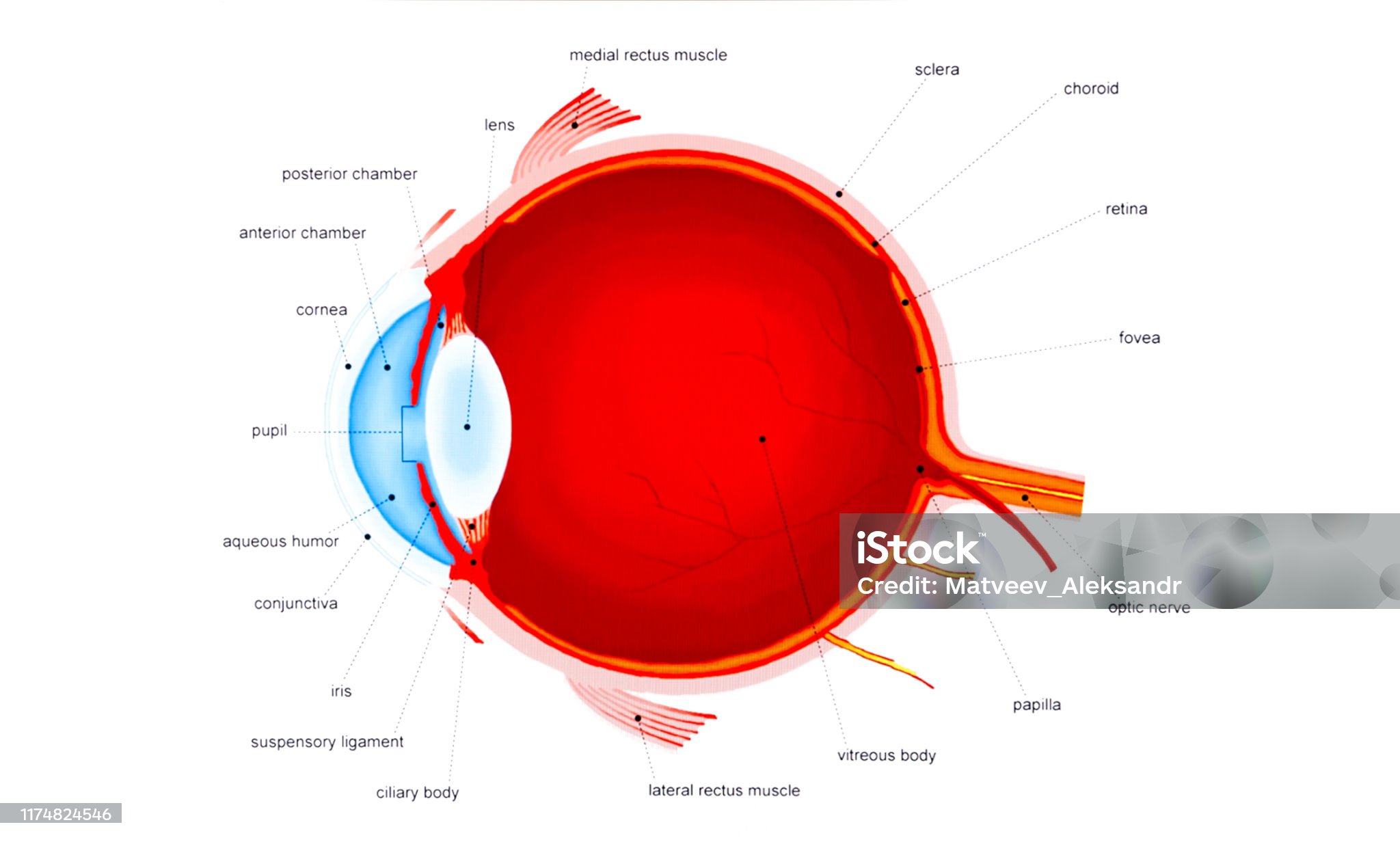
Ophthalmology is the medical-surgical specialty that studies the structure and function of the eye. Like the skin, the eye's surface is in contact with the external environment, necessitating a series of protective mechanisms. These mechanisms include the eyelids and cornea, among others, with these two being particularly problematic for individuals with EB.
Eyelids
The eyelids are movable folds of muscle and mucous skin that cover the upper and lower parts of the eye. Like any other skin surface on the body, the skin of the eyelids can also be affected, leading to blisters and erosions.
In more advanced cases, ectropion may develop, a condition in which the eyelid turns outward away from the eye, leaving the inner surface exposed and preventing the eyelid from fully closing. Ectropion occurs due to repetitive scarring that causes retraction of the eyelid skin. This condition can be very uncomfortable for the patient; when the eyelids remain partially open (a situation known as lagophthalmos), it can lead to increased dryness and other ocular problems. Patients often experience a constant sensation of a foreign body and dry eyes, which can typically be addressed through surgical intervention.
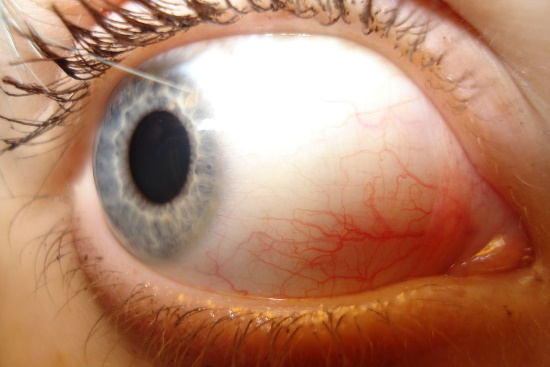
Additionally, chronic inflammation of the eyelid margins, known as blepharitis, can occur. This inflammation results from the blockage of small glands located at the base of the eyelashes, which are responsible for lubrication. The consequences include irritation, redness, and a drier eye that is more susceptible to erosions.
Cornea and conjunctiva
- Corneal Scars: When a corneal erosion becomes infected, it can result in scarring of the corneal tissue, which appears as a white spot on the cornea (corneal opacification). If the scar is located at the periphery of the cornea, it generally does not affect vision. However, if it occurs in the central area (the pupil region), it can decrease visual acuity.
- Corneal Pannus Formation: This condition involves the growth of blood vessels over the cornea, accompanied by the presence of inflammatory tissue. Without proper treatment, it can also impair vision.
- Symblepharon: This refers to the fusion of the inner surfaces of the eyelids with the conjunctiva covering the eyeball, or even with the cornea. It occurs due to the frequent formation of injuries in the conjunctiva. If the mobility of the eyeball is compromised or vision is diminished due to corneal involvement, surgical intervention may be necessary to release the adhesions.
- Obstruction of the Tear Ducts: Injuries and scarring of the conjunctiva and eyelids can lead to obstruction of the eye's drainage ducts, resulting in constant tearing due to the inability to eliminate excess tears produced for lubrication.
- Astigmatism: Scarring on the eye can cause deformities in the surface of the eyeball, resulting in abnormal curvature of the cornea and distortion of images. Prescription glasses may be necessary to correct this vision problem.