Paediatric melanoma
How is melanoma diagnosed?
Skin lesions that are suspected of being cancerous are studied via two principal methods: dermatoscopy and excision.
Dermatoscopy is a non-invasive form of examination in which a handheld tool called a dermatoscope is used to assess pigmented skin moles. It gives an excellent vision of the skin with magnification. The outer layer of our skin is transparent so that the dermatoscope allows the user to assess the patterns of the pigment in the deeper layers of the skin. Thus the experienced examiner is able to see, without surgery, the underlying structures and colours of the lesion. The practitioner, who has been specifically trained, is interested in features such as asymmetry, the pigment pattern or ‘network’ and the presence of any blue-white discolouration.

Obviously, not all moles are malignant. To distinguish ordinary/benign moles from malignant ones, doctors use the ABCDE rule. Atypical moles are studied following this guideline to have the first idea if they could be malignant or not:
Asymmetry: If you draw a line through the middle of the mole and both sides don’t look the same, it’s an atypical mole and a sign for melanoma.
Border: Benign moles have smooth and even borders, whilst malignant moles have the opposite.
Colour: Having a variety of colours/shades in the same mole is another sign for malignant moles.
Diameter: Malignant moles have a large diameter compared to benign moles. However, you can find malignant moles to be as large and have the same size as benign moles.
Evolution: The evolution or changing of a mole in your body in any shape, size, colour, elevation or any other symptom such as bleeding, itching or crusting points to danger. It is important to know and control the moles in your body, to be capable to notice if some of them have evolved and need to be re-analysed.
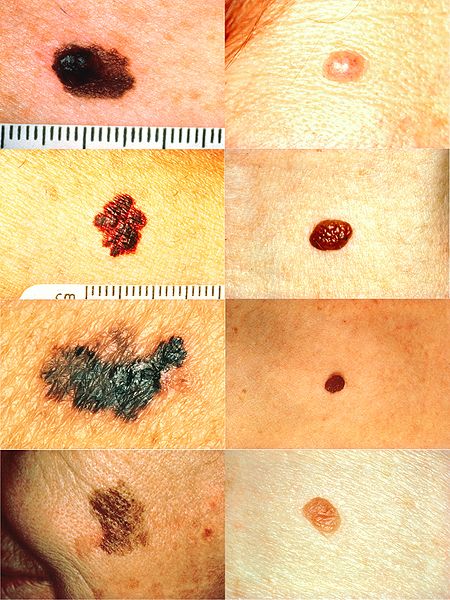
Interestingly, the ABCDE rules have been modified to include features unique to paediatric melanoma such as Amelanotic (uncoloured moles), Bleeding/bump, Colour uniformity, De novo (new moles), any diameter and Evolution of moles.9
If a skin lesion appears suspicious under the dermatoscope, an excisional surgery should be done for further evaluation. This is an invasive form of examination in which a sample of tissue is taken from the suspicious skin lesion and examined under a microscope by a pathologist to determine its abnormal cellular properties. A representative slice of the skin lesion can be taken (an incision) in order to look at the cells.
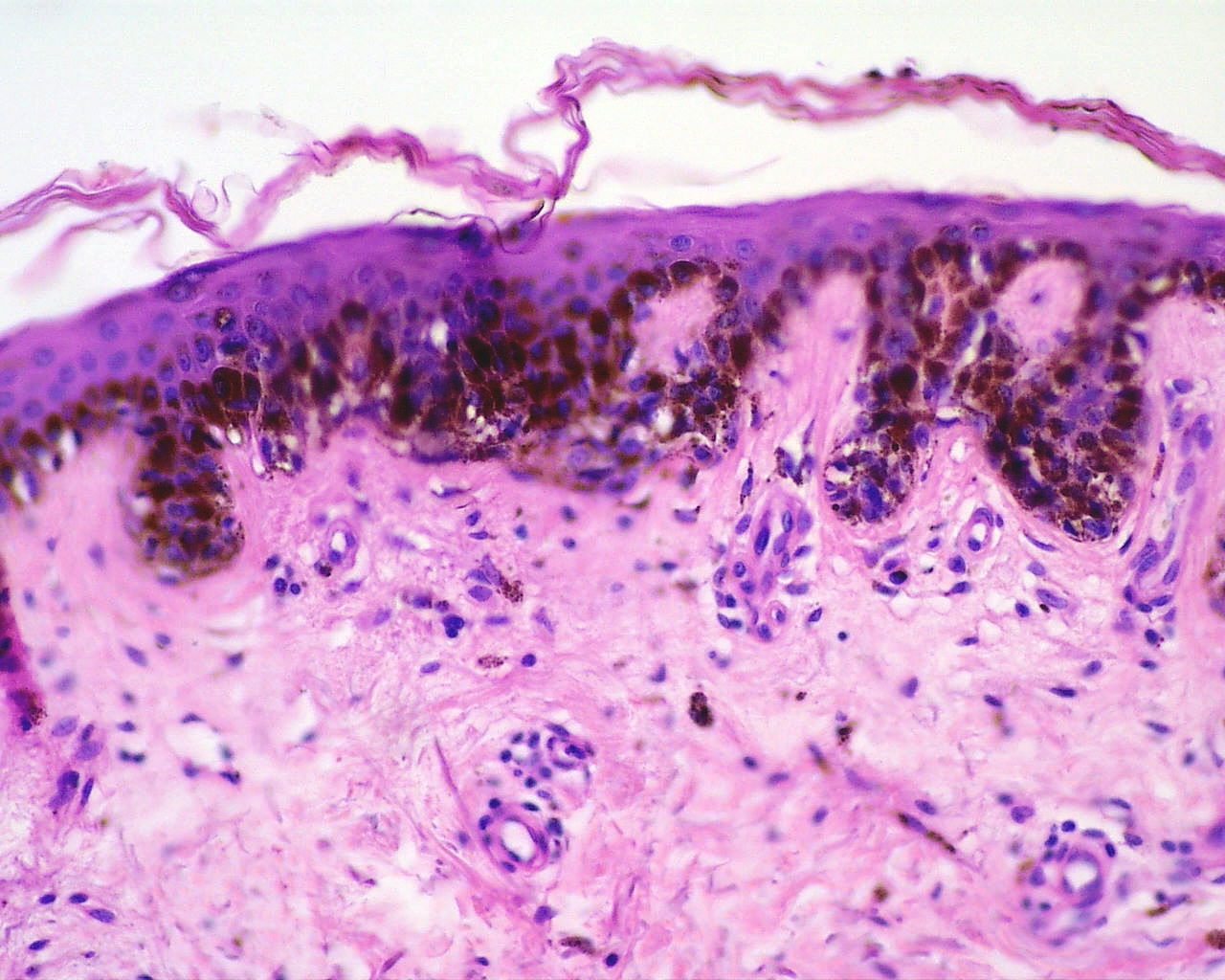
If the sample turns to be malignant, a wide local excision (WLE) must be performed and ideally accompanied of sentinel lymph node biopsy (SLNB) The depth of the tumour is essential for staging the disease and it is only by taking the entire lesion that the depth can be accurately measured. Sometimes other forms of biopsy, such as a punch biopsy, are performed to take a sample when the excision is difficult because of the location of the mole (face, hands, toes and genitals).