Gliomatosis cerebri
Gliomatosis cerebri
Gliomatosis cerebri (GC) is a very rare primary brain tumour, characterized by the diffuse and extensive infiltration of neoplastic glial cells across more than two contiguous lobes of the brain. Characteristically, it may cross the midline and affect both hemispheres. More frequently, it affects the brain, but it can also affect the brainstem and spinal cord.
GC constitutes approximately 1% of all the primary brain tumours. It can affect patients of all ages, being more frequent in adults, as is reported in published medical literature2,3. In terms of incidence, there is no clear association with sex, although some publications show a slightly higher incidence in males.4,5
In 2015, George et al.6 reviewed the literature, spanning 15 years of GC cases in paediatric populations. They described 88 patients ranging from 4 months to 21 years at the time of diagnosis, with an average age of 11.7 years at diagnosis. They also described a preponderance of boys, with a male to female sex ratio of 1.7:1.6
GC is not a histological diagnosis
The World Health Organization (WHO) 2016 histologic classification of brain tumours no longer considers GC as a distinct pathological identity. GC is therefore a clinical –a group of signs and symptoms- and a radiological –based on MRI findings- diagnosis, not a histologic one. Tumour examination must be done –as we will discuss later- and confirms the glial nature of the tumour, but does not define it.
Radiologic types of GC
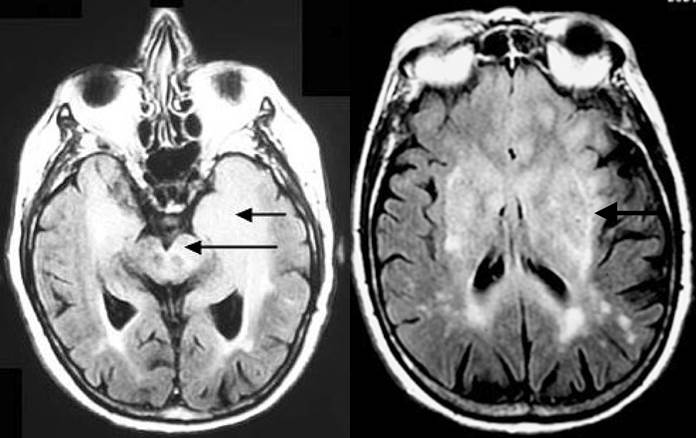
By imaging standards, GC can be divided into two types 4,7:
- Type I – infiltrates principally the white matter with no apparent mass or tumour. This is the more frequent type.
- Type II – there is a discrete tumour mass associated with the diffuse characteristic infiltrate.
GC clinical presentation
The symptoms of the disease at diagnosis are variable, depending upon which areas of the brain are affected by the tumour, the age of the patient and the growth rate. There are no specific symptoms for GC, however, most of patients present with some clinical characteristic findings4,7:
- Seizures
- Headache
- Changes in personality or behaviour
- Changes in memory or cognitive abilities
- Problems with vision
- Loss of balance or problems walking
- Fatigue, changes in activity levels
- Weakness, numbness, tingling, or changes in feeling on one side of the body
When diagnosis is suspected, a brain and spine MRI should be performed looking for the radiologic diagnostic criteria. Other rare and devastating infectious, inflammatory and degenerative conditions (i.e. acute disseminated encephalomyelitis, demyelinating diseases or progressive multifocal leukoencephalopathy) may present with similar symptoms and radiologic appearance on MRI. This makes the surgical biopsy paramount for the correct diagnosis once other conditions have been ruled out.