Epidermolysis bullosa
3.1. Pharmacological interventions
The pharmacological treatment for pain (analgesia) is usually adapted to its intensity and characteristics. It is usually started by milder medication (for example paracetamol, ibuprofen and metamizole) and it is increased by steps of analgesia, progressing until reaching more powerful medication (opiates such as morphine and its derivatives). There are also other medications called adjuvants which, although they are not specifically designed for pain management, help treating more complex pains (for example gabapentin).
In opiates (in which morphine, fentanyl or methadone, between others) it is important to know its administration is safe controlling the necessary dose being possible to controlled and progressively increase the dose until reaching the control of the pain. Usually, it is enough to use low doses and adjusted to the patient’s weight and age. The most common adverse effects to low doses are constipation and itchiness, that is why, when prescribing an opiate, it is usually advised a treatment to prevent the adverse effects. For very high doses, opiates can produce respiratory problems or even a decrease in the conscious state or delusions; however, these effects are rare and do not happen when the dose is adjusted to the patient’s conditions, starting with the minimum effective dose and increasing as needed.
It is essential to have the support of the referent healthcare team and trust their criteria, avoiding self-medication. The referent medical professional will be on charge of prescribing the most indicate type of medication according to the kind of pain suffered at each time, as well as the method of ingestion of said medication (under the tongue, by ingestion, by gastric button, through patches, through the nasal mucosa, through ointments, etc.), the dose (quantity of medication) and the number of times a day it shall be taken. Both the referent medical professional and other sanitary professionals (nurse or pharmacy personnel) can solve all the doubts presented to reduce the fear and avoid administration mistakes.
At the following, we will discuss some general recommendations to have an adequate control of the pain medications taken at home:
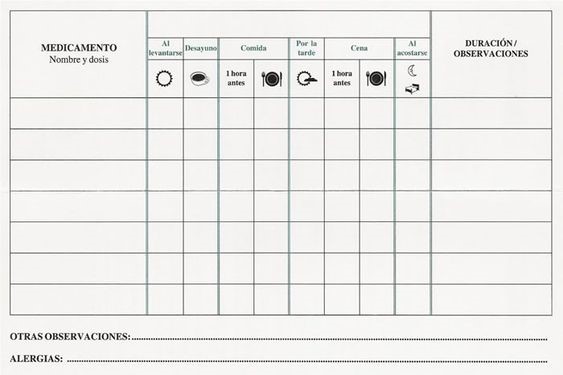
- Disposing of a listing with the medications (Figure 4). It is recommended for the health team to make it, but many times it can be made by the family themselves. It is also useful to keep the electronic prescriptions to check the type of medication, doses and frequency of the application.
- Write down and know the medications by its pharmacological name and not by its commercial one, as the latter can change between pharmacies or place where it is bought.
- Disposing of certain mobile applications to keep control of the medication, although it Is recommended to consult the reference health team before its use. Some people find useful to have alarms on their phones or writing down the prescriptions on a calendar or personal diary.
- Disposing of a clean and tidy place (first-aid kid) to keep the medication and review periodically their expiration dates.
- Disposing of a travel first-aid kit for when we are not at home (school, work, travel, trip, etc.). In the case of minors, there should be an authorized and trained adult to administer the medications if needed (Figure 5).

- Store the medications out of the reach of minors to avoid accidents.
- In case of needing syringes for the administration, make sure they are in good state, clean and with the measuring lines adequately marked to avoid dosing errors.
- Avoid mixing medications, crushing or dissolving them if we do not have the permission of the medical or pharmaceutical professional.
In the mucosal lesions (eyes, genital areas, anus, mouth, etc.) and in the wounds, localized medications can be applied, but they must still be prescribed by a health professional and the quantity and frequency of the applications must be respected.
In case of musculoskeletal and joint pain, the pharmacological approach is through anti-inflammatory treatments, but also through the preventive nutritional approach (avoiding malnutrition, administrating supplements with calcium and vitamin D to minimize osteoporosis, etc.).
- Avoid the use of medications in suppository format (through the anal mucosa) as much as possible to avoid the risk of injury.
- It is not recommended the use of topical antibiotics (in cream, drops, etc.) routinely on chronic wounds.
- It is not recommended to mix topic products.
- In case of ocular pain, the use of lubricant drops can be effective in the presence of abrasions, as well as the use of artificial tears if there is dryness. In some people with EB protective lenses have been used.
- In case of pain associated to the gastrointestinal tract, the following drugs will probably be prescribed:
- Mouth ulcers, blisters and mucositis. Oral analgesia and topical anaesthetic preparations (lidocaine, sucralfate suspension, healing gel, etc.).
- Gastroesophageal reflux. Antacid drugs, proton pump inhibitors such as omeprazole, etc.
- Oesophageal stricture and dysphagia. In addition to surgical interventions for oesophageal dilation and/or gastrostomy placement, the use of certain anti-inflammatory drugs may be useful. The use of ibuprofen should be limited due to the risk of ulcers and stomach bleeding.
- Constipation and anal fissures. In addition to treating constipation with diet, hydration and drugs, when injuries appear in the anal mucosa, topical creams with sucralfate, corticosteroids or other preparations can be applied to relieve pain and promote healing.
- Using skin products with drugs (dressing with ibuprofen, local anaesthetics creams, oral solutions with lidocaine, etc.) only under medical authorization.