Xeroderma pigmentosum
Epidermis
As stated before, the epidermis is formed by different types of cells: keratinocytes, melanocytes, Langerhans cells and Merkel cells. Keratinocytes are the most abundant cells comprising the 90% of the epidermis.3
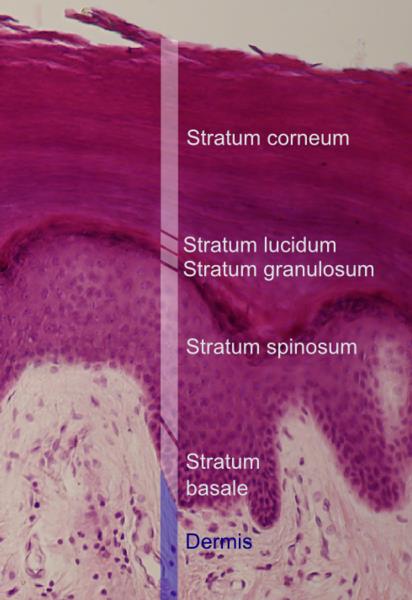
Epidermis is formed by 4 or 5 layers of cells (depending on the skin region). From the most external to the deepest layers, these are: cornified layer (stratum corneum), translucent layer (stratum lucidum), granular layer (stratum granulosum), spinous layer (stratum spinosum) and basal or germinal layer (stratum basale/germinativum). The epidermis is separated from the dermis (its underlying tissue) by a basement membrane.4
The human epidermis, which is considered a stratified squamous epithelium, is maintained thanks to the continuous division of the cells in the basal layer. The cells start to differentiate in the basal layer and continue to do so as they move towards the outer layers of the epidermis. Upon reaching the cornified layer (the most external), they lose the nucleus and fuse to the squamous layers (the multiple layers of flattened cells), which continually detach from the surface of the skin due to peeling. In healthy normal skin, the number of new cells that are produced is equal to the number of cells that breaks off.3 A cell from the basal layer needs two weeks to get to the top of the granular layer and an additional four weeks to cross the cornified layer.4 The epidermis is completely renewed every 48 days.5
This high potential of replication needs to have a genetic back-up system to minimize the number of errors made in the process of DNA duplication. One of the genetic back-up mechanisms to reduce the number of mutations caused in our skin cells is the “Xeroderma pigmentosum” group of genes. These genes have different functions in sensing and correcting the properly DNA duplication. When these mechanisms don’t work properly, they can give place to diseases such as Xeroderma pigmentosum (XP) (next section).