Kabuki syndrome
2. Insulin and sugar levels
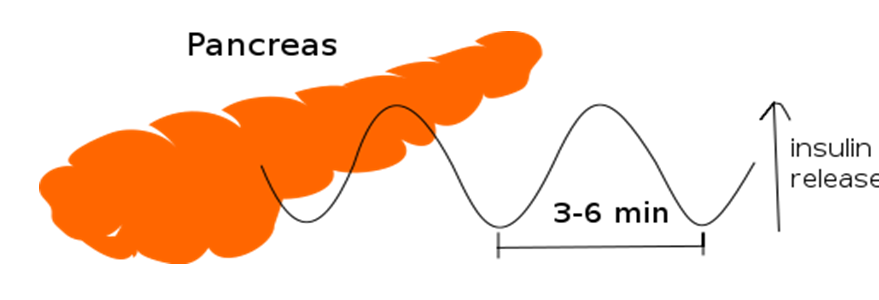
The levels of sugar (glucose) in the body are regulated by a hormone called insulin. When we consume food, large amounts of sugar enter our bloodstream. At this moment, the pancreas produces insulin, which helps to introduce that sugar into the cells of the body so it can be used as an energy source. When there is not enough insulin, as occurs in diabetes, sugar is not taken up by the cells, leading to increased blood sugar levels (hyperglycemia). Conversely, when there is an excess of insulin (e.g., insulin-producing tumors), almost all the sugar in the blood is taken up by the cells, resulting in decreased levels (hypoglycemia).
When sugar levels are very low, they can cause drowsiness or even seizures and loss of consciousness. Episodes of hypoglycemia (low blood glucose) have been reported in some patients with SK, particularly during the neonatal period. Hypoglycemia may occur in some children during the first few months of life, although it is rarer, and it is believed to be due to a combination of nutritional problems, excess insulin, and other poorly understood factors.

Hypoglycemia is diagnosed based on the presence of symptoms and by measuring blood sugar levels. Treatment consists of administering glucose orally (if the patient is able to drink), via a feeding tube or gastrostomy button, or intravenously (this should be done in a hospital).
In cases where hypoglycemia is due to excess insulin (hyperinsulinemic hypoglycemia), administration of a specific drug, diazoxide, is effective in some patients. Hyperinsulinism is likely underestimated in patients with SK and may be a presenting sign in neonates.
Failure to recognize and treat hyperinsulinism in a timely manner can lead to irreversible neurological damage and exacerbate developmental issues. It is estimated that approximately 1% of neonates with hyperinsulinism have a diagnosis of Kabuki syndrome.