Osteogenesis imperfecta
5. Fracture management
Immobilization of the affected member is one of the most extended methods when it comes to manage fractures in OI. Immobilization helps maintain the correct alignment of the bone and controll the pain in the first days following the fracture. Many bone fractures in OI are produced by low energy impacts, so the adjacent soft tissues (muscle, tendon, fat) are not really damaged (especially in fractures without displacement). This soft tissue protects the fractured bone and gives it more stability, makeing it heal faster.
The healing of the fracture in OI occurs at the same speed as in heathy people, or even faster, so the immobilization period is the same (or shorter). In addition, one of the main challenges in the management of fractures in OI is avoiding the vicious circle produced by immobilization: an immobilized bone loses bone mass, leading to osteopenia and thereby producing a greater risk of suffering a new fracture. We need to take this into account when managing fractures in people with OI: we should not immobilize the limb more time than required, and we should replace hard plaster casts with removable splints to begin the mobilization of the affected limb as soon as possible. In young children with severe OI and limited movement, some fractures may not need immobilization and light splints can be used immediately.
In addition, in patients with significant deformities in long bones, the fracture often occurs at the point of maximum bone curvature. In this case, immobilization of the fractured bone produces greater osteopenia, along with the residual deformity that appears after immobilization, setting in motion a vicious circle of fracture after fracture. Surgical treatment with intramedullary rods may help to reduce this cycle of fractures in such cases.
Intramedullary rods are metal devices (or pins) placed inside the bone. These are used to reduce the number of fractures, maintaining the bone as straight as possible and enabling that it continues growing in length. These are generally used in long bones of lower limbs (femur and tibia). Although some patients also have deformities in the upper extremities, their function is not usually compromised and they do not require surgery. This method is only indicated in cases of recurring fracture or when the deformity interferes with the function of the limb. In these cases, the bone that undergoes surgery is usually the humerus.
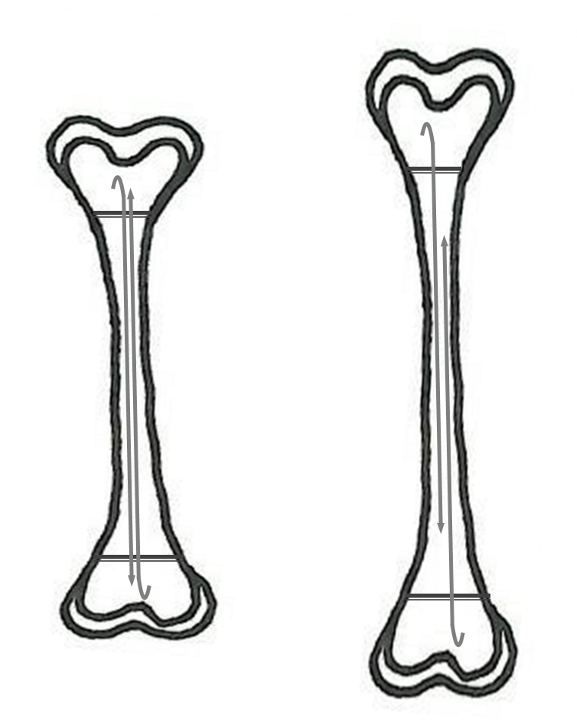
There are several types of intramedullary rods. Originally, metal (titanium) pins were used (Kirschner wires; K-wires or Rush pins), but in children, after two or three years the bone outgrows the pin, leaving part of it unprotected, giving rise to fractures and deformity. In order to minimise this possibility, it was proposed to place two pins or rods, one fixed at the proximal extreme and the other at the distal extreme. When the bone grows, these pins produce a sliding effect and no part of the bone is left unprotected (Figure 21).
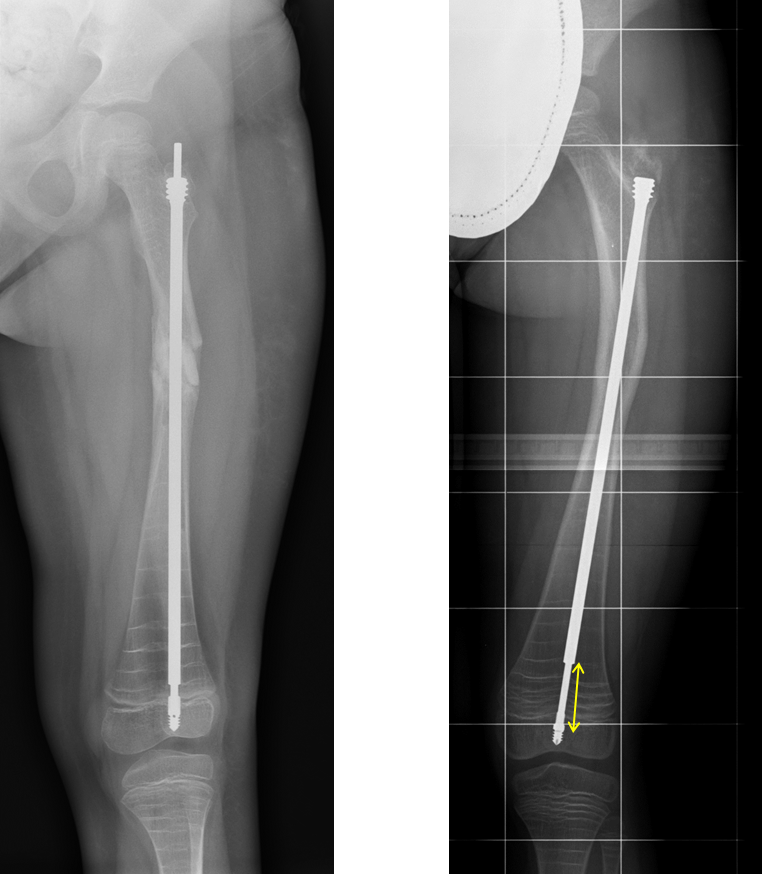
In 1963, Dubow and Bailey proposed the idea of an extensible rod, which would “grow” along with the bone. It has two parts: the “male” inside the “female”, which are progressively separated with growth. One extreme of the rod is attached to the proximal epiphysis and the other to the distal epiphysis. When the bone grows, the “male” goes out of the “female” and the rod opens up or raises like a telescopic radio antenna. Over the years, new extensible rods have been developed, offering a more secure anchoring in the epiphysis and an easier insertion into the bone. Examples of these extensible rods are the Sheffield and the Fassier-Duval (Figure 22).
There is not a single device that can ba used in all situations. The type of rod for each patient must be chosen depending on the size and characteristics of the bone (extensible rods have a greater diameter and do not fit inside the bones of very young children), the patient’s potential growth and the financial resources of the medical center.
Complications
Although rods may considerably improve the quality of life of the OI patient by providing bone resistance and, in some cases, straightening the bone, the procedure is not entirely free of complications, including the following:
- Those related to surgery: possible complications with anesthesia, bleeding, and infection.
- The device is broken or curved: this increases the smaller the rod or pin diameter is.
- Non-extension of the rod: sometimes the two parts of the extensible rod fail to slide and produce the desired telescopic effect.
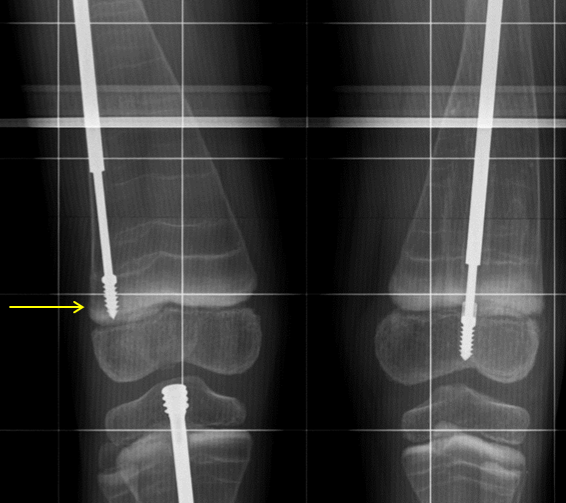
- Migration of the rod: the rod may move outside the bone. In the case of extensible rods, the anchoring to the epiphysis can be too loose, causing them to migrate (Figure 23).
- Deficient fracture healing: sometimes the bone may not heal well and an area with the fracture line may remain open for months or even years (Figure 24).
