Osteogenesis imperfecta
3. Bone mineral density
Bone mass
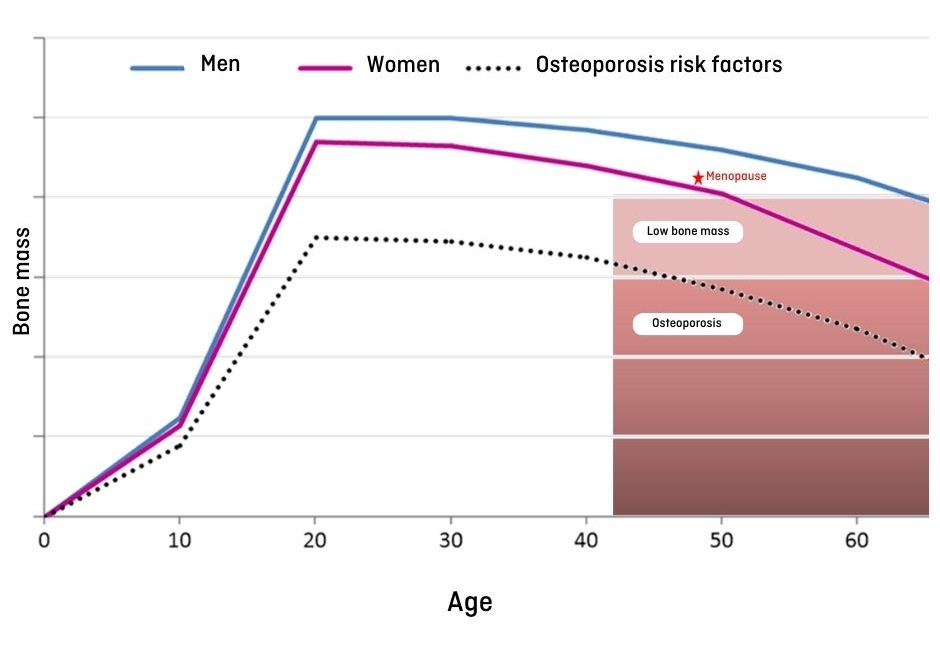
As we explained in chapter 1, the bone is a living structure made up of a collagen matrix, hydroxyapatite crystals and other proteins. The matrix is mineralised with calcium and phosphate deposits, which give it strength and its characteristic bone structure. Mineral deposition in the in bone starts at the prenatal stage, especially in the last three months of pregnancy. The bone mineral content (BMC) increases during childhood and then increases significantly in puberty, arriving at a maximum peak of bone mass at 20-25 years of age, and then it begins to decrease a progressively (Figure 8).
Factors that determine bone mass
As we have seen, childhood and puberty are crucial stages in obtaining a good bone mass. All those elements that play a role in this acquisition are risk factors for the development of osteoporosis. Osteoporosis is characterised by low bone mass and a deterioration of the microarchitecture of the bone tissue that causes increased bone fragility and, in consequence. increased risk of fracture.
Below we discuss some of the factors that determine bone mass acquisition:
- Genetic: Genetic factors are important determinants in bone mass; about 75% it depends on genetics. This is reproduced clinically in the appearance of osteoporosis in individuals with a family history of the condition, and a relationship has also been established between mutations in certain genes and the appearance of osteoporosis praecox. In addition, some genetic diseases that affect the development of the bones that may involve having osteoporosis too: osteogenesis imperfecta, Hajdu-Cheney syndrome, hypophosphatemic rickets, hypophosphatasia, etc.
- Ethnic: Probably also related to genetic factors, those of Caucasian and East Asian background have a greater risk of osteoporosis.
- Hormonal: Normal skeletal growth and development require appropriate interaction among some hormones: growth hormone, sexual hormones, steroid hormones, thyroid hormones, etc. In fact, bone mass increase during puberty occurs in parallel to the release of some of these hormones. Alteration in the secretion of these hormones, either in puberty or at other stages of development, may interfere with the correct acquisition of peak bone mass.
- Sex: Because of the action of sex hormones, women have a lower peak bone mass than men, and there is a decline of bone mass due to menopause, that does not occur in men of the same age.
- Exercise: When a mechanical force is applied to the skeleton, bone formation is activated. Exercise that applies a force to the bone, such as jumping, activates bone massacquisition, while inactivity and rest are important risk factors for osteoporosis.
- Calcium and vitamin D: Calcium is required for many body functions and it is mainly stored on the bone. It is important to ensure an adequate calcium intake in order to avoid using the calcium in the bone, as this causes its demineralisation. Calcium is obtained from the food we take (mainly in milk, dairy products and nuts). If we are not getting a minimum dose or have a risk for osteoporosis, we can take calcium as a supplement. Vitamin D is essential to the correct functioning and absorption of calcium in the intestine. Although we do get a part of our vitamin D requirement from the diet (bluefish, mushrooms, eggs, fortified dairy products), the greatest source of vitamin D is sunlight. The synthesis of vitamin D depends on the latitude (it increases when we get closer to the Equator), the pigmentation of the skin (there ia a bigger vitamin D synthesis in light-skin people), the use of sunscreen (protection factors above 8 prevent the effect of solar radiation on vitamin D), and the time of exposure (in winter there is usually a lower production of vitamin D). Vitamin D levels can be measured using blood tests, and supplements can be prescribed if levels are too low.
- Chronic diseases: Some diseases (rheumatic, neuromuscular, intestinal inflammation, anorexia, cancer,…) can produce low bone mass as a consequence of the harmful effect of inflammation on the bone, malabsorption of nutrients and physical immobility caused by the disease.
- Drugs: Corticoids, some anticonvulsants, antiretroviral drugs, heparin, chemotherapy and other drugs interfere with a correct bone mass acquisition.
- Other environmental factors, such as alcohol and tobacco, may have a negative effect on bone formation.
Measuring bone mineral density
There are several techniques to quantify bone mass. The one that is usually employed and that is optimally standardised is dual-energy X-ray absorptiometry (DXA) (Figure 9). This method consists in the emission of two types of x-rays with different energy levels, which helps to distinguish the bone from adjacent soft tissue. Bone mass is calculated measuring the degree of attenuation of the rays produced by the bone. With the current devices we can obtain high-resolution images with low radiation levels.
Bone mineral density is the parameter that is most commonly used to assess bone mass and is expressed as grams per square centimeter (gr/cm2). The value obtained is compared with tables that contain normalised values for the general population, and then a standard deviation (SD) is calculated (that is, how different the patient’s value is from the average value for the general population):
- In adults, we use the T-score, which is the standard deviation with respect to the average peak bone mass in healthy young adults of the same sex (compared to the maximum value for bone mass). Based on the T-score, patients are then classified as: 1) Normal: between +1SD and -1SD; 2) Osteopenia: between -1DS and -2.5D; 3) Osteoporosis: the value is lower than -2.5DS.
- The T-score is not used for paediatric patients, since it refers to the peak bone mass in an adult population, and children have not reached this peak yet. In children and adolescents, we use the Z-score, which is the standard deviation with respect to healthy children of the same age and sex. A Z-score is considered normal when it is between +1DS and -1DS, but in order to diagnose osteoporosis in children, there has to be a bone mineral density with a Z-score below -2SD associated with the presence of fractures (if there are no fractures, we talk about low bone mineral density for that specific age). Another thing to bear in mind is that, in patients with low stature or retarded growth, as is sometimes the case with OI, we must correct the Z-score making an adjustment for the patient's height.
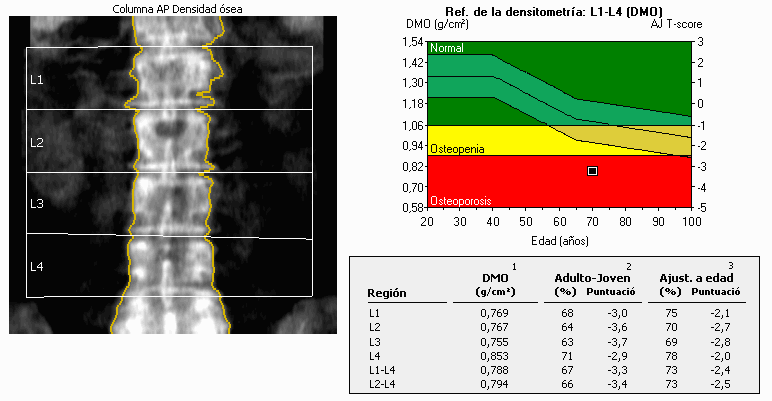
We can measure bone mass with DXA at different points of the skeleton. The most common parts in adults are the backbone and the hip, and in children we can do the measurements in the whole body except for the head.
Densitometry is a highly standardized technique in adults, available in many medical centres and widely used for the diagnosis of osteoporosis, which is a common pathology in adults. However, as we have seen, we must bear in mind certain considerations when using this procedure with children (use of the Z-score, points for measurement, adjustment for height), which means the procedure should be done by specialised radiologists to avoid interpretation errors.
In OI, bone mineral density is usually decreased (although in some cases it may be normal), and a periodic use of densitometry is useful to provide follow-up and assessment of the response to treatment (which usually shows an increase in bone density). The presence of metal objects such as pins and column support rods that some OI patients may have can interfere with the calculation of bone mass in the densitometry, and this must be taken into account when evaluating the results.

Quantitative computed tomography is another technique used to assessment bone mineral density. It has the advantage of providing information concerning the volume of bone in three dimensions (while DXA densitometry is limited to two dimensions) and it is able to distinguish cortical from trabecular bone. On the other hand, it involves greater radiation and there are fewer reference values. Although new high-resolution tomography is being developed its use is still not standardised for OI and it is limited to specific cases and research.
Ultrasound, which has the advantage of emitting no radiation, has been used in adults to assess bone density in hands and feet, but it also has its limitations, as it cannot be used for the backbone or for deep bones such as the femur. In paediatrics, it is not widely used in normal clinical practice. It is rather used as a research tool and as a complement to DXA densitometry.
Other techniques under development for the assessment of bone density include nuclear magnetic resonance and bone vibration analysis.