Hereditary retinal dystrophies
1. Stargardt disease
The most common juvenile macular dystrophy. It occurs with a progressive loss of the photoreceptors in the macular region, which causes a reduction in central vision. The estimated prevalence according to Orphanet is 1-5/10,000 cases.
Symptoms begin in the first or second decade of life with a variable progression over time, with reduced central vision and preservation of peripheral vision. In some cases, the onset of symptoms in adulthood or after the patient's seventh decade of life has been described, due to the deterioration of the macula associated with age. In this research project, pediatric patients will be preferably studied, or those who, as adults, had a debut of the disease before coming of age or in the closest years.
The symptoms of the disease are characterized by a progressive loss of central vision that causes blurred vision and, sometimes, an increasing difficulty adapting in the dark. Peripheral vision is usually normal. Most affected individuals also have colour vision problems. The alteration of the cones is what causes the problems related to daytime vision. Patients complain of reading difficulties, sometimes blind spots in their vision and, in advanced stages, impaired colour vision. Sometimes patients may have photophobia.

The course of the disease as well as the severity of visual loss is highly variable among individuals. It is very rare for a patient with Stargardt’s disease to become totally blind, although some can reach legal blindness.
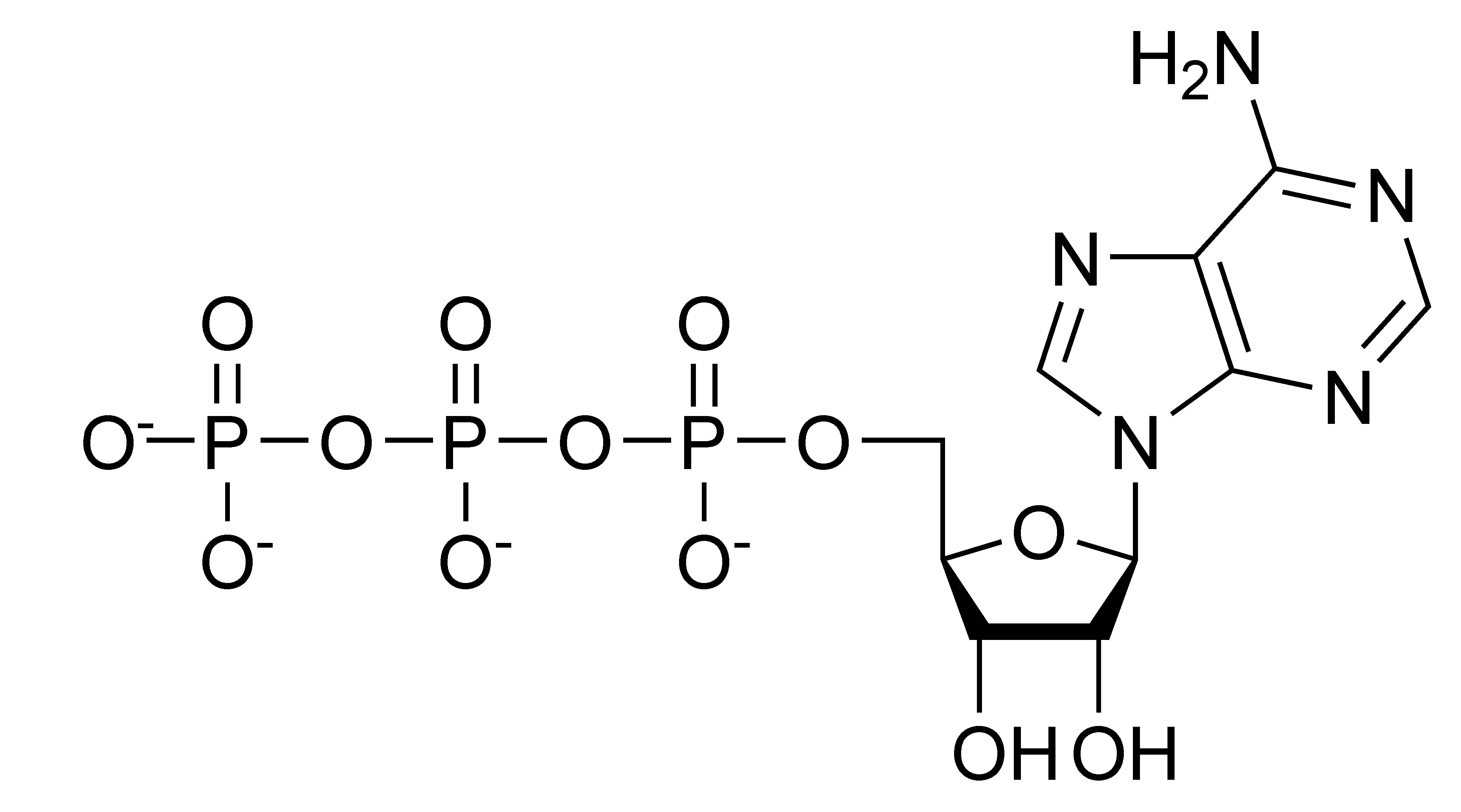
The main gene affected by the disease is the ABCA4 gene, which encodes adenosine triphosphate (ATP), a fundamental nucleotide in the correct DNA coding and which is expressed directly in the configuration of the rods and cones of the retina. When ATP is not encoded correctly, defects occur in the photoreceptors and in the pigment epithelial of retinal cells (RPE), ultimately causing RPE cellular death and subsequent loss of photoreceptors.
Nevertheless, forms with dominant inheritance have also been described, caused by mutations in the STGHD4 gene or in the PROM1 gene. It has also been recently associated with other genes.
Clinical diagnosis is based on ophthalmologic examinations consisting of visual acuity and visual field tests, ophthalmoscopy, electroretinogram (ERG), fluorescein angiography (FA), eye fundus autofluorescence (FAF), and optical coherence tomography (OCT), which reveal macular abnormalities (progressive atrophy) and spots in the central macula but can also extend beyond the vascular arcades. Fluorescein angiography reveals the characteristic dark choroid in approximately 85% of patients. The diagnosis can be confirmed by genetic testing of the ABCA4 gene.
Differential diagnosis includes multifocal pattern dystrophy simulating STGD1 and retinal and/or macular dystrophies such as central areolar choroidal dystrophy (CACD), achromatopsia, cone dystrophy (CD), and cone-rod dystrophy (CRD).
Prenatal diagnosis is technically possible but is not used in clinical practice, except for confirmed family history in which genetic counseling is performed.
Due to the high clinical variability, the prognosis depends on certain parameters (in particular, age of onset and electroretinographic findings) that can help the clinician to calculate an indication of the evolution of the disease. Stargardt's disease can progress rapidly over a few months or gradually over several years leading to a severe decrease in visual acuity. Peripheral vision is usually unaffected, although some patients may progress to a cone-rod phenotype that does not affect peripheral retinal function.