Exercise in neuromuscular disorders: a moving topic

Impact of neuromuscular diseases on education and working opportunities of patients and carers
Nicole Voet is a rehabilitation physician and scientific researcher in the Rehabilitation Centre Groot Klimmendaal in Arnhem and in the academic medical hospital Radboud University Medical Centre in Nijmegen, the Netherlands. During her study of medicine, she spoke out the wish to help people with a chronic disease by exercise and she is nowadays making her dream come true. Her PhD research was about the effect of cycling exercises and cognitive behavioral therapy (CBT) on experienced fatigue in facioscapulohumeral muscular dystrophy (FSHD), the third most common muscular dystrophy worldwide with an estimated prevalence of one in 8,000 people.
FSHD, fatigue and physical activity
FSHD is an autosomal dominant disorder affecting primarily the muscles of the face and the shoulder girdle, but later in life many muscles of the trunk and the extremities can become affected. To date, there is no curative treatment available for FSHD. As a consequence, although life expectancy is normal, 20% of the patients become wheelchair-bound due to muscle weakness. In addition, more than 60% of FSHD patients experience chronic fatigue and, with that, a lower level of social participation. Physical inactivity has shown to be the most important perpetuating factor of fatigue in patients with FSHD. However, being physically active is difficult for patients because of muscle weakness, which may lead to a vicious circle of fatigue and inactivity. Both rehabilitation interventions of Nicole Voet’s PhD project showed a positive effect on fatigue and the level of physical activity in patients with FSHD. After CBT, the level of social participation increased. Unexpectedly, after both interventions, there was a deceleration of the increase of fatty infiltration in the leg muscles: both interventions are able to decelerate the progression of the disease.
FSHD and exercise: the patient’s perspective
Nikolas Fahlskog, Swedish by nationality, is married with two young children (2 and 7 years old) and works full time (sometimes more) as a freelance innovation & marketing consultant, in Amsterdam. He was diagnosed with FSHD in its right shoulder at age 20 during his military service. Before and after the diagnosis he has maintained a very active life practicing many different types of sports on competitive level, mainly skiing, sailing, kayaking, rowing and biking. Some precautions are taken with regards to avoiding heavy backpacks, but except for that he continues to live an active life as much as time permits.
A few years ago, Nikolas witnessed his father loose strength rather quickly in his lower back and its otherwise very strong posture. As a consequence, he has been forced to reduce or modify a lot of activities in his life in different ways, like skiing, kayaking, hunting and general work around the house and forest. The diagnosis of Nikolas father is also FSHD, something that had previously not been diagnosed despite tests when Nikolas was diagnosed many years before. This quick deterioration of Nikolas father’s back strength triggered Nikolas to consult the Dutch healthcare system to get more advice on how to prevent FSHD to spread. This led Nikolas to meet Nicole and they both share the same belief and passion for exercise as a medicine, which has led to further collaborations.
What research on exercise and FSHD tells us
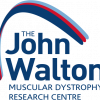
Although increasing the amount of physical activity is an essential part of CBT for fatigue in FSHD, both scientists and clinicians are astonished about this beneficial effect. “Is fatigue all in the mind?” and “How can a psychological treatment achieve an effect at a muscular level?” are frequently asked questions. The answer to these questions is that a part of the solution is, in fact, literally “in the mind”. Psychological factors such as illness cognitions coping style and level of acceptance of the disease are known to be strongly correlated with the degree of social participation in patients with a muscular disease. It is noteworthy that these correlations, comparable with the level of experienced fatigue, are relatively independent of the degree of physical impairments. This is also called the “disability paradox”: having physical impairments has little influence on the degree of social participation. This paradox can be explained by the perceived burden of disease in patients with FSHD. As shown in Figure 1, muscle weakness is not only just an indirect perpetuating factor of experienced fatigue; it also constitutes a relatively small part of the experienced burden of disease. Fatigue, pain, sleep disorders and physical inactivity determine the majority of the experienced burden of disease in FSHD and MD1. This implies that psychological interventions are not only able to improve the level of experienced fatigue, but can also improve the degree of social participation and mood of patients with a muscular disease, even when there is a progression of the disease.
Encouraging FSHD patients to exercise
Nicole loves exercising too: she practiced fin swimming on a high level (2nd place in the World Championships) and currently practices triathlons. She always tells her patients that they are top athletes in daily life and therefore have to live like top athletes: alternate short periods of rest and activity, eat healthy food, do not smoke and aspire to a good sleep quality. However, this advice can be more easily followed by top athletes than by FSHD patients. Patients with FSHD frequently have a job, have to care for their kids and have household activities to face.
Nicole met Nikolas when he was searching for advice to restart his exercises after an accident, in which a truck hit him during cycling. He broke his right shoulder, the shoulder in which he had relatively less strength because of his FSHD. They soon noticed that they both had the same dream, which resulted in the webinar, but both are also working together on a network of care for neuromuscular disorders. This network has the goal to achieve a better quality of life for neuromuscular patients by connecting patients, caregivers, physicians, therapists, patient organizations and all other relevant stakeholders together. The network will also help to bring the positive effect of exercise to patients.
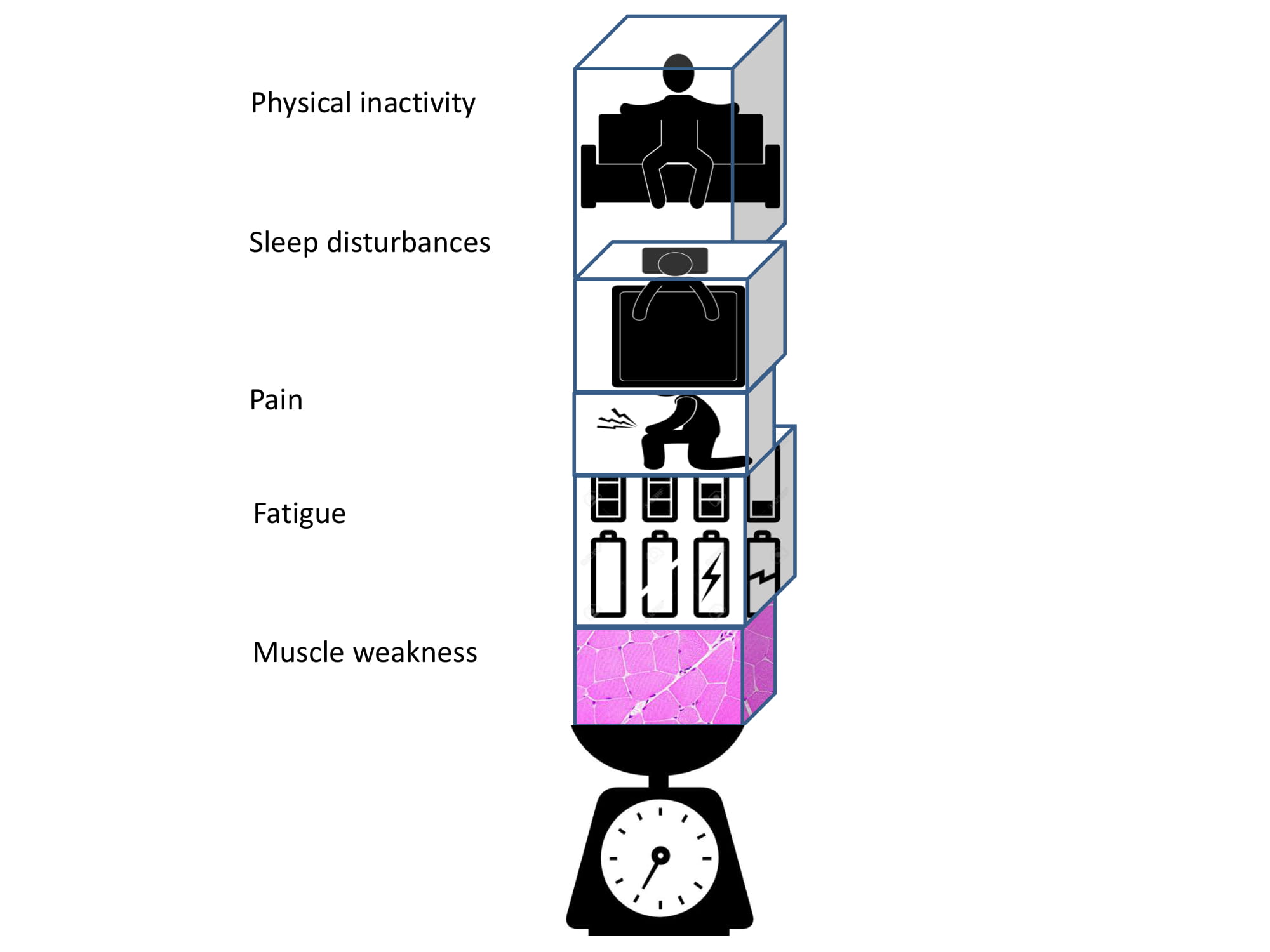
Many patients with FSHD are captured in a vicious circle of inactivity (see Figure 2). Due to fatigue, patients often alter their lifestyles and reduce their activities. Low physical activity levels may lead to even greater weakness and atrophy of skeletal muscles, which causes a vicious circle of disuse and weakness. Physical inactivity in turn can lead to chronic cardiovascular and muscle deconditioning and increased cardiovascular health risks.
It is important to break this circle with training and encouraging an active lifestyle, especially in patients with no cardiac or pulmonary co-morbidity, such as in patients with FSHD. In the past, clinicians were reluctant to prescribe exercise to patients with FSHD. They often referred to possible muscle damage due to overuse. However, this hypothesis has never been supported with thorough research. What proved to be impossible in drug trials up to now did succeed in research using behavioral and exercise interventions. In FSHD, aerobic exercise training as well as CBT did not only reduce the degree of disease burden, but also established a beneficial effect at the muscular level probably as a result of increased physical activity: exercise as medicine!
Listen to the full webinar on Exercise in Neuromuscular Disease here.
