Osteogenesis imperfecta
3. Inheritance in OI and reproductive options
Types of inheritance
Inheritance is the capacity to transmit the information that we carry in our genes to our offspring. Each gene is expressed in two copies, or alleles, one coming from the father and the other from the mother. The final expression of a gene will be the result of the interaction of the two alleles.
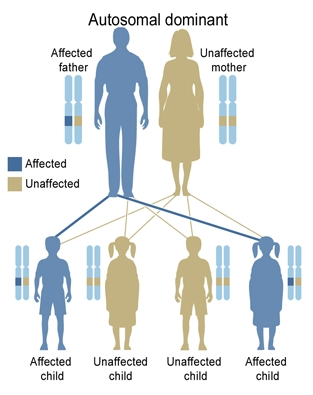
We speak of autosomal dominant inheritance of a disease when a mutation in one of the alleles of a gene is able to give rise to that disease (Figure 13). In the case of children, if they have a copy of the mutated gene they will be affected, and if they have two copies of a non-mutated gene they will be healthy. The genes COL1A1, COL1A2, IFITM5 and P4HB are inherited in an autosomal dominant way. When OI is caused by a dominant mutation, the gene may be inherited from one of the parents or it may be the result of a new mutation that took place at the time of conception (a so-called de novo mutation). As these de novo mutations are stable changes in the DNA of the child, they can be inherited by their future offspring.
In a few cases the mutation may not be present in all the cells of the body (what in genetics is known as mosaicism). When an egg and a sperm join, they form a single cell known as a zygote. This cell then divides, creating different cell lines that become differentiated in the tissues of the organism. Mosaicism occurs when a mutation appears in this process of cell division (Figure 14); from this point onward, only the cells deriving from this mutated cell will carry the mutation and give rise to a mosaic individual.
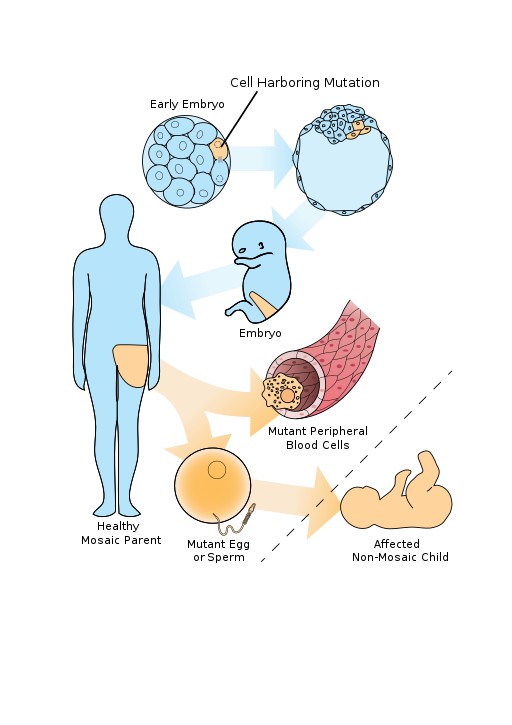
In some cases, the individual does not have the symptoms of the disease, but if the mutation is present in their sex cells it may be transmitted to the next generation (Figure 15). In this case, it may appear as if there is a de novo mutation, because the parents are apparently healthy but have an affected child, but if we carry out a genetic study in the parents with modern techniques we will be able to detect the mutation in a small proportion of their cells.
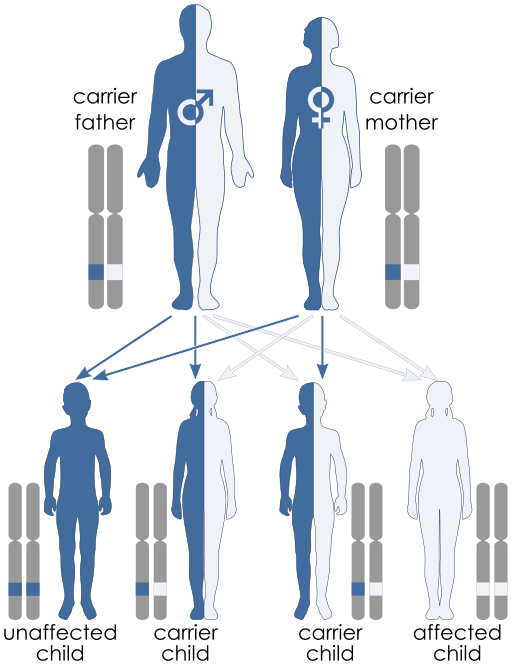
In autosomal recessive inheritance we need two copies of the mutated gene for the disease to be developed (Figure 16). When there is only one mutated allele, the individual is a carrier but does not develop the disease. For the child to have the disease, both parents would need to be carriers. A child with two mutated alleles will be affected while a child with two alleles that are not mutated will be healthy. In OI, mutations in the genes SERPINF1, CRTAP, P3H1, PPIB, SERPINH1, FKBP10, BMP1, SP7, TMEM38B, WNT1, CREB3L1, SPARC, PLOD2, SEC24D, P4HB and NBAS have an autosomal recessive pattern.
If the patient presents the same mutation in the two alleles, we say the mutation is in homozygosis. If, on the other hand, the mutations are different, each of them is in heterozygosis. In diseases inherited in a recessive way, the patient must to present two mutations, one in each allele of the gene, in order to develop the disease. For this reason, we may find patients with two equal mutations (in homozygosis) or with two different mutations (both in heterozygosis) in the same gene. In the case of autosomal dominant diseases, the affected patient has only a single mutated allele (mutation in heterozygosis).
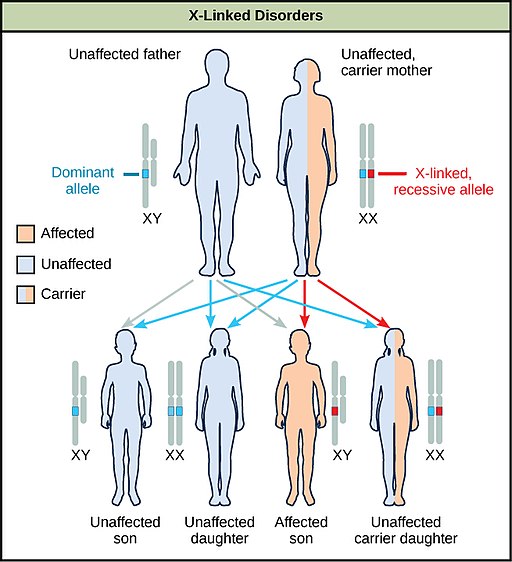
Chromosomes X and Y determine biological sex. Sperms may have an X or a Y chromosome, while the egg always have an X chromosome. If each the egg and the sperm have an X chromosome, the foetus will be a girl (XX genotype). On the other hand, if the sperm has a Y chromosome, and then fuses with the egg, the foetus will be a boy (XY genotype). When the gene that causes the disease is located in the X chromosome, we say it is a sex-linked inheritance or chromosome X-linked inheritance (Figure 17). In the case of males (XY genotype), we must recall that they only have one copy of the X chromosome —that is, a single copy of the gene. This is why, in general terms, in the case of sex-linked inheritance males are usually healthy when the allele of the X chromosome is correct, and affected when the allele is mutated. Females may be carriers of the disease when they have a mutated copy of the gene located on the X chromosome while the other is healthy. In OI, mutations of the MBTPS2 and PLS3 genes cause the disease via a sex-linked inheritance pattern.
Reproductive options
OI has a wide spectrum of severity, with severe forms causing perinatal death and others that offer a life expectancy similar to that for healthy people, but with hospitalisations, frequent paediatric controls, intravenous treatment and a substantial family and social burden.
This is why given the possibility of a new pregnancy, the parents of a child with OI may need specialised genetic counselling, in order to be fully informed of their reproductive options.
1. Prenatal diagnosis: a set of procedures employed to study the foetus in the first weeks of pregnancy. If the foetus is affected, a voluntary interruption of the pregnancy could be considered. In order to carry out a prenatal diagnosis, we need to know beforehand which mutation the child has, and we also have to do a genetic study of the parents. There are two ways to obtain a sample from the foetus:
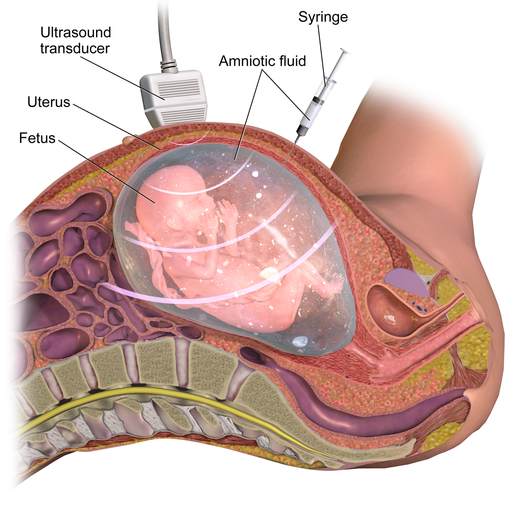
- Amniocentesis: it is generally performed at weeks 16 to 18 of the pregnancy. Amniotic fluid is obtained trans-abdominally (through the abdominal wall of the pregnant woman). This is the most common method, as there is very little risk of losing of the foetus (1%) and the results are highly reliable, as it is very unlikely that the sample gets contaminated (Figure 18).
- Chorion biopsy: this is generally done at weeks 11 to 14 of the pregnancy. It may be trans-abdominal (through the abdominal wall of the pregnant woman) or trans-cervical (via the vagina). The advantage over amniocentesis is that the extraction is done earlier in time, but it is an invasive technique that involves taking a sample of the chorionic villus via a catheter, so there is a greater risk of foetal loss (2-3%).
Following a prenatal diagnosis made with a study of the foetus in the early weeks of pregnancy, if the foetus is affected then a voluntary interruption of the pregnancy may be considered. However, if parents decide to continue with the pregnancy, having a prenatal diagnosis allows a more specific follow-up of the pregnancy, the delivery, and the post-natal period.
2. Preimplantation genetic diagnosis: allows the identification of genetic defects in embryos in vitro, in the laboratory, before their are transferred to the uterus. Embryos are studied individually and only those that are not affected with the disease are implanted. This process has several stages:
- A cycle of patient preparation involving hormonal stimulation, ovulation induction and collection of the oocytes through an ovarian puncture. A single sperm cell taken from the father is injected into each gamete (oocyte) taken from the mother.
- From that moment, cultivation of the embryos begins. When a certain number of cells have been formed (3 to 5 days) the embryo is analysed to identify the possible mutation.
- Once the genetic study has been completed, those embryos that are not affected by the disease are transferred to the uterus of the mother (one or more, depending on each individual case).
3. Gamete donation (egg cell or sperm cell): another option to avoid developing the disease is to ask for a donation of a gamete from a healthy person. We will choose sperm or egg donation depending on which parent is affected by the disease or mutation. If there is an egg donation, the egg from the donor is fertilised with the sperm of the father, and then the fertilised egg is transferred to the uterus of the mother. In the case of sperm donation, we carry out an artificial insemination: sperm from the donor is injected into the uterus of the mother-to-be.