Osteogenesis imperfecta
2. Eyes disorders in OI
There is a great variability of ocular manifestations in osteogenesis imperfecta. In this chapter we will review some of these pathologies. With the exception of the presence of blue sclerae, most of the ocular manifestations we will describe are rare in OI and can also be seen in individuals not affected by OI.
1. Alterations at the level of the sclera
As we have seen, the sclera is the outer layer of the eye, which under normal conditions is thick and white in colour, and has a protective role for the eye. It is a layer very rich in collagen fibres. The presence of blue or greyish coloured sclerae is a common finding in some OI subtypes (Figure 4). It is thought that the reduction of collagen fibres at the level of the sclera leads to a decrease in its thickness and increases transparency, allowing the uvea, the middle layer of the eye (which is highly vascularised and darker in colour) to become more visible. Although it is very rare, cases have also been described of patients with OI in whom the sclera has ruptured (spontaneously or due to trauma), exposing the uveal layer.

2. Alterations at the corneal level
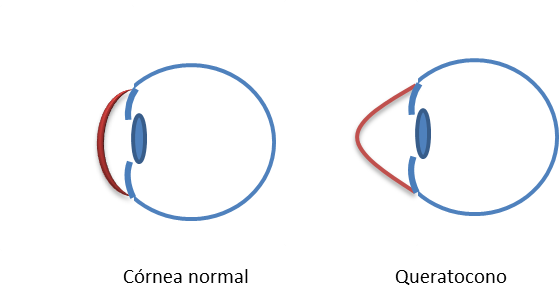
As with the sclera, the cornea in OI may also be thinner. Another finding seen in OI patients is keratoconus, which is a progressive disorder in which the cornea takes on a conical shape, due to a thinning of its centralmost part and a progressive increase in corneal curvature (Figure 5). This results in distortion of vision leading to astigmatism and myopia. In mild cases, vision can be corrected with glasses or contact lenses. In more severe cases, surgery or even corneal transplantation may be necessary.
Even less common is the presence of a keratoglobus, which is a diffuse thinning of the cornea, resulting in globular protrusion of the entire cornea. There is a risk of corneal rupture with minimal trauma.
Finally, alterations in the diameter of the cornea can also be observed: both corneas with a reduced diameter (smaller) and with an increased diameter (larger, also called megalocornea). In this situation, refractive errors such as myopia or astigmatism, and sometimes lens subluxation (the lens is displaced from its usual position), are also usually associated.
3. Alterations at the level of the crystalline lens
Cataract is the loss of transparency of the lens of the eye (opacification), which hinders the passage of light and can lead to visual impairment. Cataracts occur frequently with age in the general population and can also be seen in patients with OI, although it is not known how often. Treatment in cases of significant vision loss consists of surgical removal of the lens.
Also with age, the lens becomes less elastic and loses the ability to change shape to focus on closer objects. This is called presbyopia or eyestrain. It appears in most people with age and also in patients with OI.
4. Intraocular pressure changes and glaucoma
In glaucoma, damage to the optic nerve leads to a decrease in the visual field. There are different types and causes of glaucoma, but the main risk factor for developing glaucoma is increased intraocular pressure (IOP). Glaucoma occurs in 1-2% of the general population over 40 years of age, being more frequent in certain ethnic groups, and has also been associated with individuals with OI, although incidence figures are unknown. Its association with OI could be related to changes in the corneal anatomy of some of these patients; or to disorders in the lamina cribrosa, which is the opening of the sclera through which the optic nerve fibres enter; or even to alterations at the level of the trabecular meshwork, through which the aqueous humour drains.
Glaucoma treatment is generally focused on reducing IOP. It may include oral medical treatment or eye drops or surgical procedures to try to re-establish a balance between the formation and elimination of aqueous humour to control ocular pressure.
5. Other ocular alterations
Less frequent findings such as vitreous or retinal haemorrhages, retinal detachment or optic nerve disorders have also been described in individuals with OI.
Strabismus, which is the loss of parallelism of the eyes, so that each eye looks in one direction, causing ocular deviation, is a relatively common ocular finding in the general population and may also occur in OI. The presence of strabismus during childhood can lead to amblyopia or lazy eye, and reduced visual acuity in the affected eye.