Epidermolysis bullosa
1.2. Pathophysiological bases
Itching can be caused by chemicaltransmitters or by physical or thermal stimulation, that is, it can be caused by changes in temperature, tissue injuries or the production of different substances in the skin (histamine, prostaglandins) due to various causes.
There are 4 structures implicated in the itch generation:
- Keratinocytes: these are the cells that make up the outer layer (epidermis) of the skin.
- Skin defence cells: they increase in areas of skin injury (wounds, burns, infection) to help repair and heal.
- Peripheral nerves: these are the structures (similar to telephone wires) that carry sensations of itching or pain from the skin to the central nervous system (spinalcord and brain).
- The central nervoussystem: made up of the spinal cord and the brain, which is where the sensation of itching is received. It usually interprets this sensation and gives an order to scratch or relieve this itch with some action.
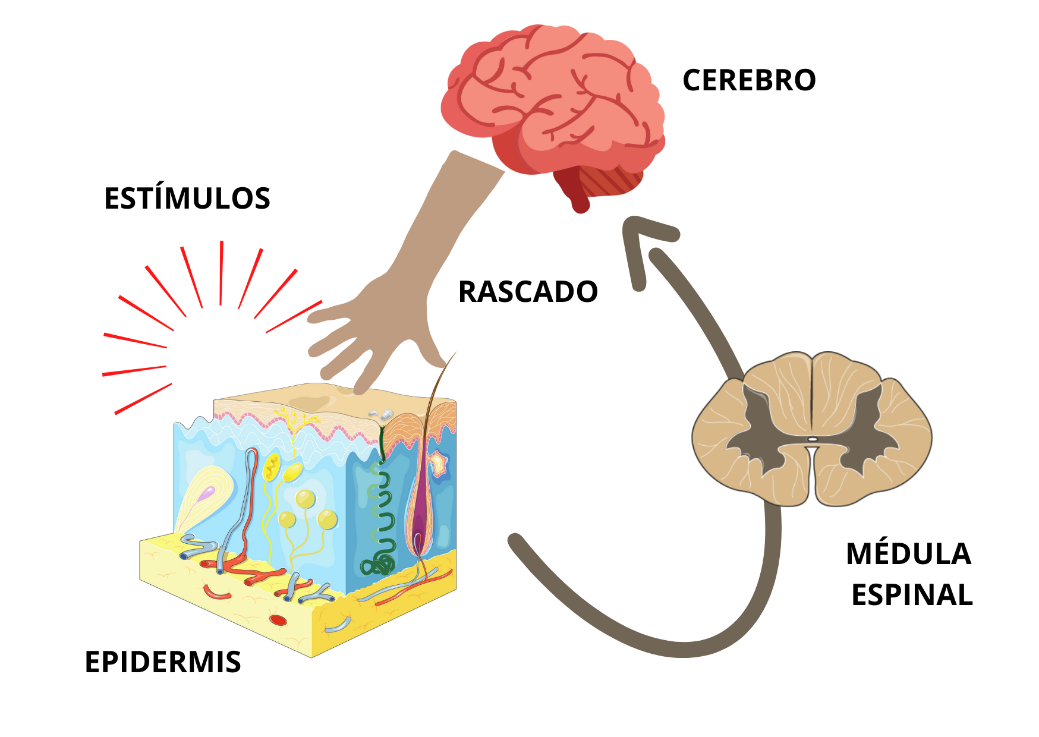
In the following figure, the nervous circuit by which the itchiness is perceived is illustrated (Figure 2):
When the itchiness become chronical, there are more implicated factors, and the approach gets more complicated. The continuous skin inflammation and the persistent nerve activation to transmit the itchiness sensation make the brain become sensitive to the itchiness, in other words, it perceives it even easier. Also, in people with recurrent, long-term injuries in the skin the end part (most superficial) of the skin nerves gets damaged, so they do not function properly and the itchiness sensation becomeschronic.
In patientswith EB, the pathophysiological causes of itching seem to be slightly different and include more factors. Although the mechanisms are not entirely clear, some aspects of the disease itself may be influencing the presence of itching:
- Multiple wounds in varying degrees of healing. Healing wounds and the skin around them are more pruritic (itchier) than intact skin. This may be due to the increase in skin defence cells in the first moments of healing, which are also usually more abundant in chronic wounds. These defence cells produce inflammatory molecules (the prostaglandins that have been previously mentioned). Prostaglandins stimulate nerves in the skin, initiating and perpetuating itch signals. This has also been observed in patients with large burns.
- Role of the fibers of the epidermal nerve. RDEB patients with high rates of pruritus have been found to have significantly reduced and disorganized nerve fibers in the skin compared to healthy people. Although the cause of these alterations is uncertain, repetitive skin injury and compositional disruption in the secondary extracellular matrix or collagen VII defects could be influencing EB itch.
- Altered skin barrier function. In pruritic skin there is usually a dysfunction of the barrierfunction of the skin. This dysfunction results from modifications in the genetic expression, which could make the skin vulnerable to pruritic factors in the environment (such as heat or humidity) and lower the itch threshold.