Juvenile dermatomyositis
1. Specific myositis antibodies
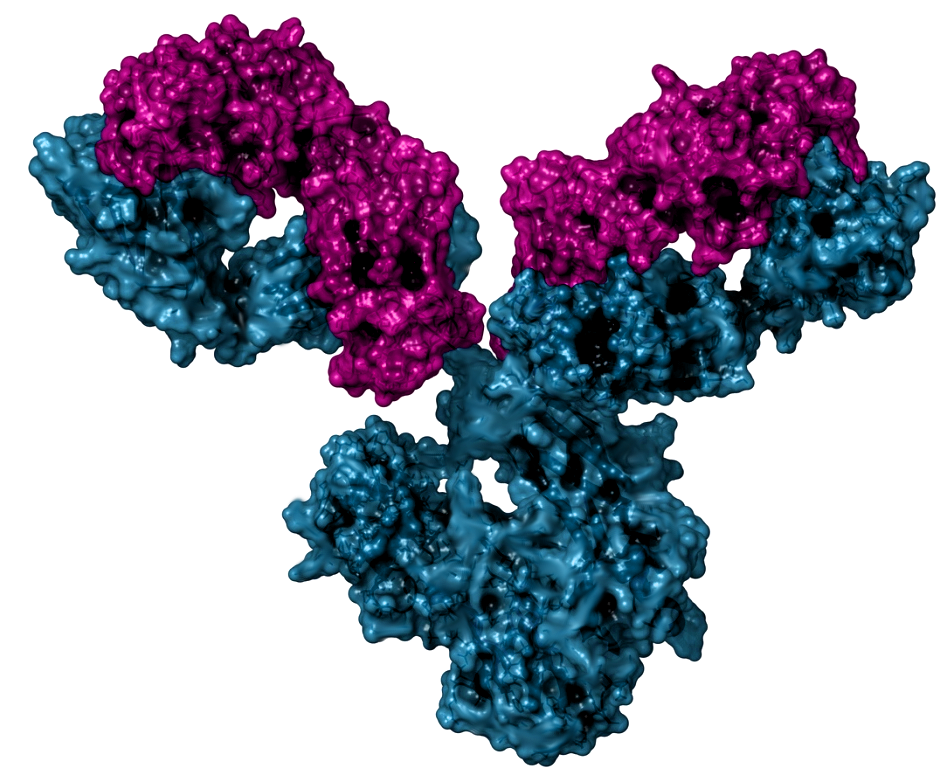
An antibody (also called immunoglobulin) is a protein found in the blood and other tissues, created and developed by our immune system, which acts against what we call antigen (an element that the body recognises as something foreign and foreign to us, usually a part of a bacterium or virus). In this case, this antibody mistakenly recognises a part of our body as an antigen and acts to our own detriment, causing inflammation and other lesions, giving rise to what we call autoimmune diseases. Antibodies that act against antigens in our own body are called autoantibodies.
JDM, considered an autoimmune disease, is related to the presence of some of these autoantibodies. Although their presence is not necessary to diagnose the disease, they can help in the typing and monitoring of the patient (knowing which symptoms the patient is most at risk of presenting, knowing the evolution, prognosis...). In fact, the literature increasingly supports the association between these antibodies and the clinical characteristics of patients.
Antinuclear antibodies (ANA) are the best known autoantibodies, and although their determination is not indicated for the diagnosis of JDM, they are usually performed in the baseline analysis to make the differential diagnosis with other diseases such as systemic lupus erythematosus.
Two types of autoantibodies can be detected in patients with inflammatory myopathy: myositis-specific antibodies, present almost exclusively in patients with inflammatory myopathies, and myositis-associated antibodies, present in patients with inflammatory myopathies and in patients with other connective tissue diseases (Table 1).
| Myositis-specific antibodies | Myositis-associated antibodies |
|---|---|
| Anti-Jo1 and other antisynthetases | Anti-U1-, U2-, U3- and U5-RNP |
| Anti-Mi-2 | Anti-PM-Scl |
| Anti-Signal Recognition Particle | Anti-Ku |
| Anti-p155/140 (TIF-1) | Anti-Ro |
| Anti-MJ (NXP-2) | Anti-SUMO/RAE |
| Anti-CADM-140 (MDA5) | Anti-43KD (cNIA) |
| Anti-200/100 (HMG-CoA reductase) |
Autoantibodies are detected in approximately 70% of patients with JDM. Characteristically, in patients with inflammatory myopathies there is no overlap between the different types of autoantibodies. The most frequently found myositis-specific antibodies in JDM are anti-p-155 and anti-NXP2. The patient phenotype varies depending on the autoantibody detected (Table 2).
| Anti-p155 (anti-TIFF-gamma) | Severe skin disease, generalised lipodystrophy, chronic course of disease. |
|---|---|
| Anti-MJ (anti NXP2) | They tend to have more weakness, more frequent GI involvement with bleeding and ulcers, and calcinosis. Only 8% of these patients will be in remission 2 years after starting immunosuppressive treatment. |
| Anti-MDA5 | Less muscle involvement (hypomyopathic), interstitial lung disease and arthritis. |
| Anti-Mi2 | Typical dermatomyositis rash. Unlike in adults, they are not associated with a shawl sign or cuticular hypertrophy. |
Other myositis-specific antibodies, rarely found in JDM, are anti-synthetase, anti-SRP and antiCADM-140 antibodies. The presence of anti-synthetase antibodies is associated with an increased risk of lung disease.
The prognostic role of muscle biopsy in JDM seems to be conditioned by the patient's autoantibody profile. Thus, it would have no prognostic value in patients positive for anti-MDA5 or anti-Mi2 but it would have prognostic value in the rest of the patients, so that the higher the pathological anatomy score, the lower the probability of being in remission 5 years after diagnosis.