Juvenile dermatomyositis
Others
1. Skin lesions
Approximately 90% of patients with JDM present with typical and disease-specific skin lesions known as Gottron papules and heliotrope erythema.
- Gottron's papules or Gottron's sign (57-91%): erythematous-violaceous, raised lesions, sometimes associated with desquamation, located symmetrically on bony prominences. They frequently appear on the small joints of the hands although they can also appear on knees, elbows, ankles and/or small joints of the feet (Figure 1).

- Heliotrope erythema (66-87%): violaceous-purpuric lesion on upper eyelids. It may be associated with palpebral swelling (eyelid edema) and/or malar rash. If the inflammation and erythema appear asymmetrically or with different coloration, other diagnoses should be considered.
The presence of at least one of the two typical skin lesions is by definition necessary to confirm the diagnosis of dermatomyositis. The location of the lesions is important for the diagnosis, since both heliotrope erythema and Gottron papules appear in typical locations already mentioned above.
Photosensitivity is present in 50% of patients.
Other skin lesions may appear simultaneously:
- Periungual erythema (35-91%): redness of the skin adjacent to the nail base (Figure 2). Present in up to 90% of patients. The nail bed can be studied by a technique known as capillaroscopy, which consists of using a lens and a light to assess the characteristics of the periungual capillaries. In JDM these capillaries may be decreased in size or altered in morphology although there is no specific pattern for this disease. The capillaroscopy pattern may become normalized in patients with only one episode of disease (monocyclic course).
- Cuticle overgrowth: frequently associated with periungual erythema (Figure 2).

- Facial erythema, local or generalized: Typically appears in areas of sun exposure. Occasionally it may be itchy. It may be localized at facial level (42-100%), on the trunk, nape of the neck, shoulders and upper third of the back (shawl sign, 19-29%) or on the extension surface of the extremities. Dilated capillaries (telangiectasias) and/or alteration of the thickness and characteristics of the skin (poikiloderma) can be seen over the erythema. Scalp involvement may be associated with capillary loss. In the most severe cases, edema (inflammation) may be associated.
- Mucosal lesions (35%): dilation of oral mucosal capillaries and/or oral aphthae (Figure 3). Present in up to 40% of children.

- Inflammation of the subcutaneous cellular tissue (panniculitis): clinically manifested as cutaneous nodules usually painful.
- Cutaneous ulcers (5-30%): reflect severe skin disease. They may appear on the inner canthus of the eyes, axillae, elbows or on pressure surfaces (Figure 4).

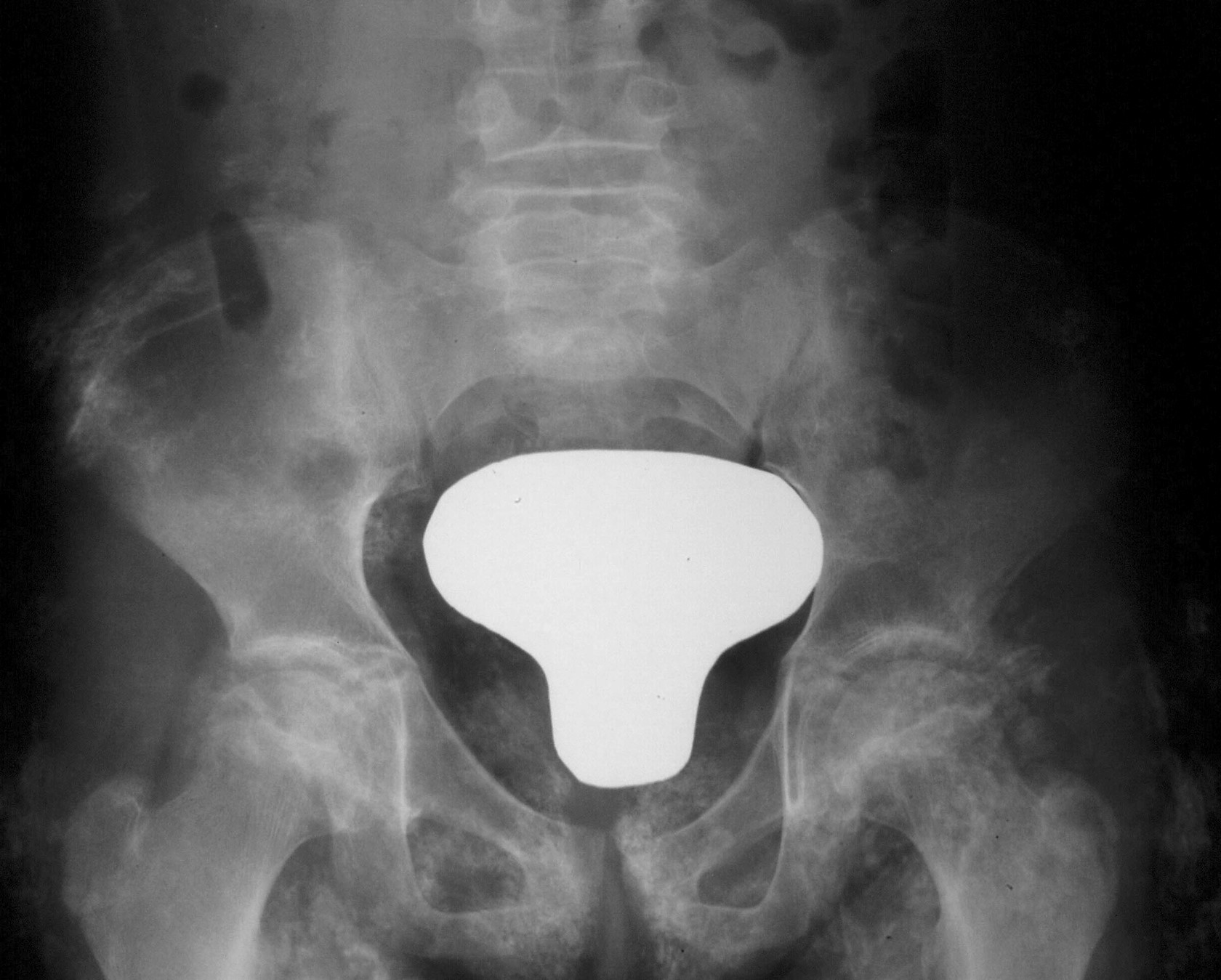
- Calcinosis (3-34%): calcium deposit in skin, subcutaneous cellular tissue and/or muscle clinically manifested as nodular lesion and/or plaque of hard consistency (Figure 5). Present in up to 40% of patients, they frequently appear during evolution, associated with poor disease control and/or delayed diagnosis. They can be associated with inflammation and can be painful. One of the main complications is the superinfection of the lesions. Sometimes they drain liquid content to the exterior.
- Lipodystrophy (4-14%): progressive loss of fat and subcutaneous cellular tissue, partial or generalized (Figure 6). It can appear in areas of previous panniculitis. It is sometimes associated with metabolic alterations such as increased triglyceride levels or insulin resistance.

Last modified
05 October 2023