Juvenile dermatomyositis
3. Complementary tests to evaluate muscle damage
1. Blood analysis:
The assessment of certain markers in the blood allows us to indirectly evaluate muscle damage. Regardless of the cause of this damage, substances that are normally inside muscle cells will be released into the bloodstream and can be determined in a blood test. These substances, known as muscle enzymes, are proteins that assist in normal muscle function. We can determine the value of different enzymes such as creatinine kinase (CPK or CK), lactate dehydrogenase (LDH), aspartate aminotransferase (GOT or AST), alanine aminotransferase (GPT or ALT) or aldolase. The levels of these enzymes do not correlate with the severity of the disease and even when the disease has been evolving for months, their value may be normal. Therefore, they are not considered an optimal tool for patient follow-up.
2. Electromyogram:
The electromyogram (EMG) is an electroneurophysiology test that assesses the electrical activity of the muscle. The contraction of a muscle is due to the electrical discharge of the nerve that controls it. Depending on whether the nerve, the muscle or the junction between the nerve and the muscle (neuromuscular junction) is affected, the characteristics of the electrical impulses transmitted vary.
The test is performed with the patient seated or lying on a stretcher. It consists of stimulating the different muscles to be evaluated with an electric current transmitted through a needle inserted into each muscle. This test allows us to determine the origin of the muscle weakness (nerve, neuromuscular junction or muscle) but not its cause.
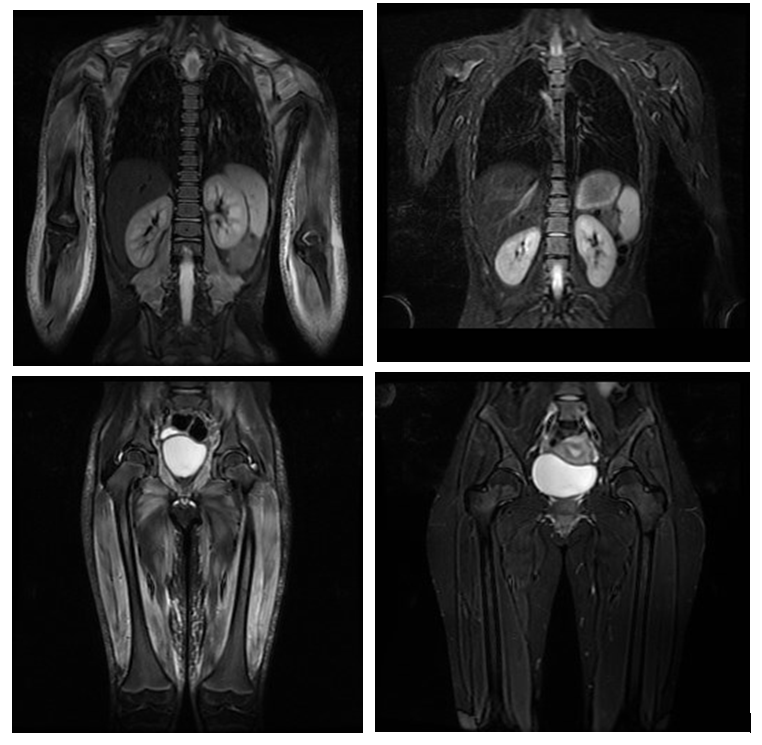
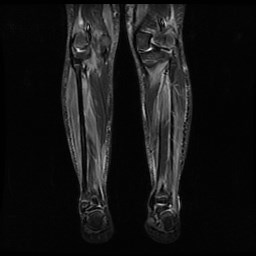
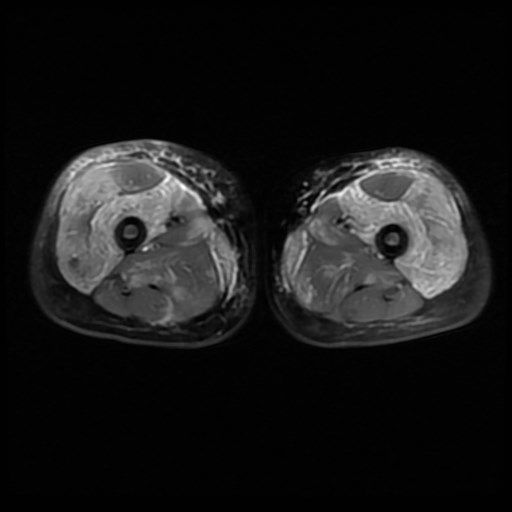
3. Muscle magnetic resonance imaging:
Magnetic resonance imaging (MRI) is a diagnostic imaging test that allows indirect assessment of the presence of muscle inflammation. It is performed with the patient lying down, requiring that the child does not move during the time in which the images are taken. It does not radiate, does not require the administration of contrast, but the usual duration is 30-45 minutes so that, in cases of younger age may be necessary sedation of the patient. It can be performed on a specific area of the body or the whole body, allowing us to assess the extent of the inflammation. The MRI has allowed us to verify the involvement of muscles that were initially thought to be respected, such as the distal muscles of the extremities (further away from the trunk). We can therefore affirm that JDM is a predominantly but not exclusively proximal myopathy.
It allows us to assess muscle, fascia and subcutaneous cellular tissue and to detect inflammation in clinically unaffected muscles. It is an objective test that allows differentiation of activity from muscle damage and that normalizes with treatment, making it a useful tool in patient follow-up. It also has prognostic value, as a relationship has been described between the involvement of the subcutaneous cellular tissue and the development of calcinosis.
The main problem is that at present there are no standardized sequence protocols or a single resonance assessment scale. Different research groups are working in this direction in order to homogenize clinical practice.
4. Muscle biopsy:
It consists of taking a fragment of muscle tissue in order to observe it under the microscope. It is normally performed in the operating room under anesthesia to avoid pain. Normally the quadriceps or deltoid is chosen but the choice of muscle can be modified depending on the MR images, in order to increase the cost-effectiveness of the sample. It is best to avoid muscles that have been stimulated during the electromyogram so that the sample is not artifactual (spoiled) and to use appropriate surgical material to try to ensure that the sample obtained is of the best quality for evaluation under the microscope.
Once the sample is obtained it must be processed in the laboratory. After this, different sections will be obtained on which different stains will be applied in order to evaluate the structure of the muscle fibers and the presence of inflammatory cells. Muscle biopsy, although not necessary for the diagnosis of JDM, allows us to confirm that we are dealing with an inflammatory myopathy and it is advisable to perform it whenever there are diagnostic doubts. Furthermore, at the present time, different research groups are trying to identify prognostic factors in the muscle biopsy at diagnosis, which could help us to estimate the evolution and/or response to the available treatments.
5. Biomarkers:
The search for biomarkers arises from the need to detect the presence of subclinical activity (not associated with symptoms), which could be related to a subsequent relapse or appearance of damage associated with the disease. At present these markers are not used in clinical practice as they are still in the research phase. Mainly work is being done on the determination of biomarkers in peripheral blood.